
Alejandro Spiotta (Medical University of South Carolina, Charleston, USA) outlines what he believes could be the next frontier in cerebral aneurysm care—artificial intelligence (AI)—and the specific benefits it holds in this space.
Endovascular treatments for brain aneurysms and other cerebrovascular diseases have significantly improved over the past few decades, and continue to progress at a very fast pace. From advances in techniques to improvement in medical devices, to growing expertise, the future is looking promising for both aneurysm patients and the physicians providing their care.
AI integration holds great promise to be perhaps the biggest disruptor in recent medical history. Emerging technologies, such as AI-based image interpretation tools, are spurring further this rapid progression. These technologies are well-established in helping physicians save time and improve patient care by automating the clinical and operational aspects of ischaemic stroke management and will soon be applied to aneurysm management.
Unruptured intracranial aneurysm remains a major public health concern, affecting 6.5 million people in the USA, or one in 50, according to the Brain Aneurysm Foundation. Accurate, early diagnosis is critical and, unfortunately, misdiagnosis or delays in diagnosis occur in up to one quarter of patients when initially seeking medical attention—making these advancements all the more important.
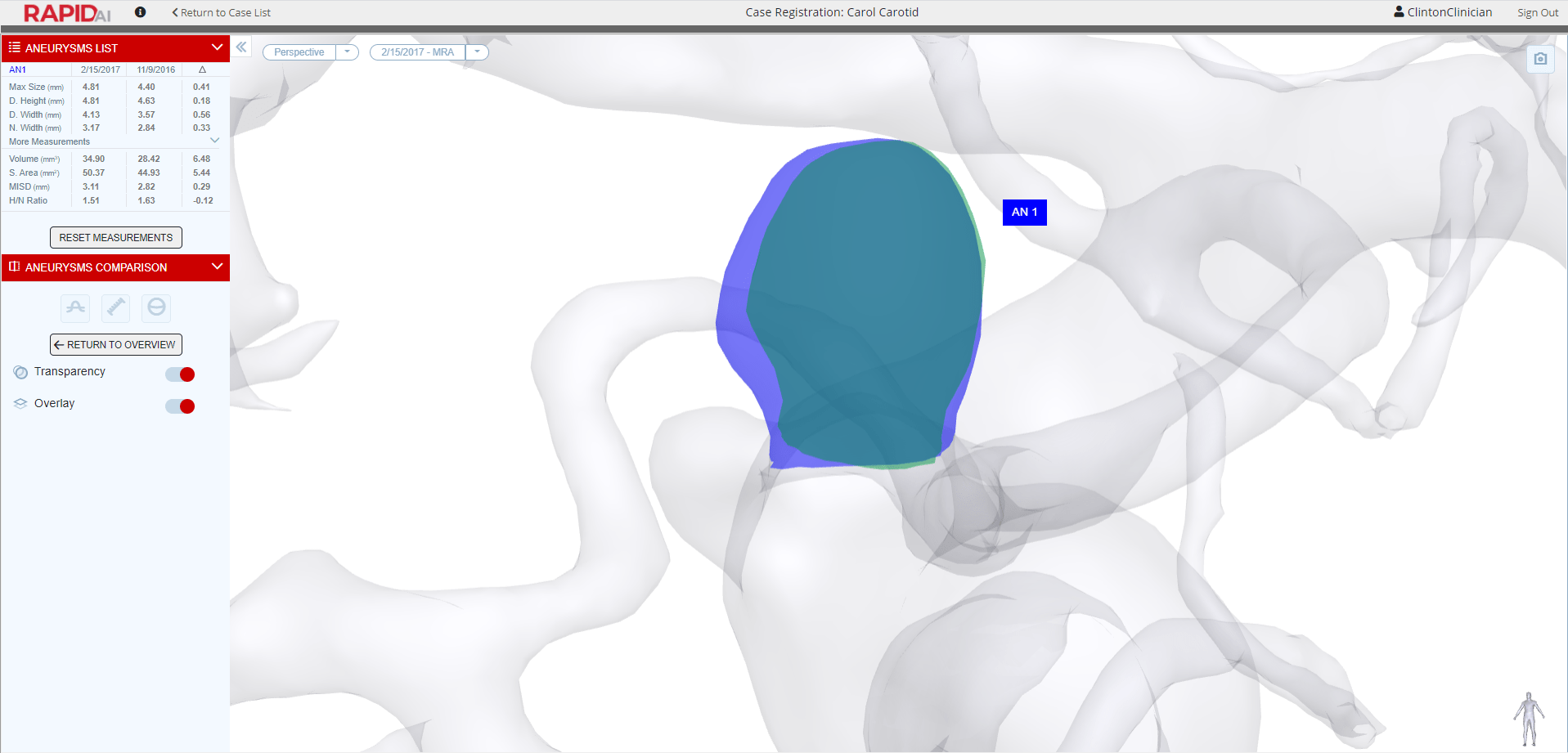
AI technologies can support and augment the process of identifying and monitoring intracranial aneurysms by increasing sensitivity of detection as well as standardising quality across centres so that every patient benefits from the highest possible diagnostic yield. Magnetic resonance angiography and computed tomography angiography (CTA) scans paired with integrated AI tools can enhance the ability of a physician to find aneurysms by increasing their sensitivity, as a recent study demonstrated.1 The study found that AI capabilities helped junior radiologists match the performance of more senior radiologists in identifying the most challenging aneurysms (<5mm) on CTA. AI incorporation was also found to improve workflows by reducing time to diagnostic reporting.
From an operational standpoint, these technologies are showing tremendous promise in helping hospital teams eliminate workflow inefficiencies and manage a higher capacity of case volume by taking over tedious tasks, and streamlining and standardising processes. The goal of these tools is to reduce communication breakdowns by connecting multidisciplinary staff involved in the management of aneurysm patients. Effective workflow applications should also be able to advance communication among doctors and nurses by allowing them to update each other in real-time through text messaging and automated status updates—minimising the number of phone calls. Although reducing workflow inefficiencies in the emergency department is far from easy, integrating machine learning platforms can offer relief and ultimately result in more consistent, quality care.
Given the great promise to improve detection and workflows for monitoring and treating aneurysms, what is preventing widespread adoption of AI among the healthcare community? First—and of utmost importance—the data supporting its use, including transparent sensitivities and specificities at various anatomical locations and in various conditions (including in the presence of subarachnoid haemorrhage, for example), must be made available to promote physician trust in the technology.
Another barrier is lack of resources. Implementing new technologies requires time, training, and budget. There must be tangible, widespread results on improvements to patient outcomes, care times, cost-savings, and positive physician feedback to ensure a successful return on investment. These metrics are often challenging to prove upfront to garner the necessary support from hospital administration. Another barrier is clinician resistance, or hesitation, towards emerging technologies. Many times, physicians remain faithful to legacy systems they have used for years and have difficulty modernising. It is critical to reinforce that emerging technologies will not replace physicians entirely, but rather help them do their jobs more effectively and efficiently to better serve their patients.
Although every aneurysm case reveals its own unique set of clinical and operational challenges, emerging technologies have the power to offer significant improvements to care. As hospitals more widely deploy modern solutions, the healthcare ecosystem as a whole will benefit as it continues to advance into new territories. Health systems should actively seek out new solutions to recurring problems and not be skittish to push the boundaries of innovation. I believe the coming wave of AI-based technological improvements will profoundly and forever more alter the way we as physicians interpret images (see), communicate across large healthcare systems and interact with patients (speak and hear), and ultimately treat (touch) diseases.
Advancements like these are being supported by the Stroke Thrombectomy and Aneurysm Registry (STAR) collaboration, led by the Department of Neurosurgery at the Medical University of South Carolina (Charleston, USA).2 The STAR registry serves as a multicentre initiative to track, and ultimately improve, patient outcomes after stroke thrombectomy or endovascular aneurysm treatment using large patient cohorts and compiling expertise from experts across the globe. It also provides a platform for physicians to share their experiences and learn from one another.


References:
- Wei X, Jiang J, Cao W et al. Artificial intelligence assistance improves the accuracy and efficiency of intracranial aneurysm detection with CT angiography. Eur J Radiol. 2022; 149: 110169. DOI: 10.1016/j.ejrad.2022.110169. Online ahead of print.
- MUSC. 2022. STAR (Stroke Thrombectomy and Aneurysm Registry). [online] Available at: medicine.musc.edu/departments/neurosurgery/star. [Accessed 10 March 2022].
Alejandro Spiotta is a professor of Neurosurgery and Neuroendovascular Surgery, division director of Neuroendovascular Surgery, and programme director of the Neurosurgery Residency Training Program, in the Department of Neurosurgery at the Medical University of South Carolina (MUSC) in Charleston, USA.
DISCLOSURES: Spiotta has either received research grants from or provides consulting for Medtronic, Penumbra, RapidAI, Siemens, Stryker and Terumo.













