A new study has found stent-assisted endovascular techniques with Acclino stents (Acandis) are a feasible treatment for complex intracranial aneurysms. Reporting in the Journal of Neurointerventional Surgery (JNIS), the authors report that even in challenging complex bifurcation aneurysms they achieved good treatment results using the kissing-Y stenting technique.
In a retrospective review, Friedhelm Brassel and colleagues from the department of Radiology and Neuroradiology, Sana Kliniken Duisburg, Duisburg, Germany and the department of Diagnostic and Interventional Neuroradiology, Medical School Hannover, Hannover, Germany, identified 43 patients with various intracranial aneurysms treated electively with stent-assisted endovascular techniques by using at least one Acclino stent between June 2012 and October 2015 with a follow-up until April 2016.
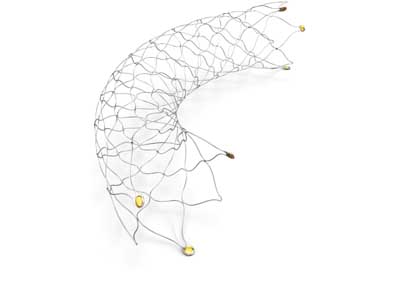
In the study two different types of Acclino stents were used— the 1.9F stent system and the newer Acclino flex stent system. The stents are self-expandable nitinol microstents with a closed-cell design. The stent system features three radiopaque markers at the proximal and the distal end of the stent, indicating correct position and expansion of the stent. The three transport wire markers allow increased visibility and a safe and precise placement of the stent. The distal end of the transport wire has a highly flexible atraumatic soft tip.
The Acclino flex stent system is the third generation of closed-cell stents from Acandis. “The new optimised asymmetric cell design ensures an improved vessel wall apposition even in tortuous vessels. Both later generations of stents are available with 3.5mm and 4.5mm diameters, each of them with five different stent lengths (15mm, 20mm, 25mm, 30mm, 35mm), allowing a broad range of vessel sizes from 1.5mm to 4mm to be treated. Sequential coil embolisation of the aneurysm can often be performed without changing the microcatheter after stent deployment. The stents are retrievable and repositionable if an adjustment of the stent is necessary, even if the stent was deployed between 50% and 90% of its total length,” the authors explain.
Thirty-six of 43 aneurysms treated were complex wide-necked aneurysms. The other seven were dissecting aneurysms. Sixteen patients were treated with two or more stents. Eleven of these patients with a complex bifurcating aneurysm were treated with the kissing-Y stenting technique. The aneurysm distribution was as follows: 14 at the anterior communicating artery (AcomA), eight at the basilar artery (BA), seven at the intracranial ICA, five at the middle cerebral artery (MCA), five at distal vertebral artery (VA) segments, two at the anterior cerebral artery (ACA), one at the posterior inferior cerebellar artery, and one at the posterior cerebral artery (PCA). The mean aneurysm size was 7.7×5.8mm (range 2–17mm).
The mean follow-up time was 11 months. Post-procedural angiograms were obtained immediately after coiling of the aneurysm and all patients underwent post-interventional cranial CT directly after the intervention. The patients’ first follow-up was performed at three to six months. The second follow-up was carried out one year later. Post-interventional angiograms and follow-up MR angiography and DSA were reviewed and evaluated based on the Raymond−Roy Occlusion Classification (RROC) by two experienced interventional neuroradiologists in consensus.
“We report no stent migration or fracture during the follow-up. In three of the 36 wide-necked aneurysms we performed no coiling or incomplete coiling, due to vessels arising out of the aneurysmal sac. For this reason, we excluded those three aneurysms from the statistical assessment using the RROC. For the remaining 33 wide-necked aneurysms, complete occlusion in post-procedural angiograms was achieved in 30 (91% RROC 1) cases. We observed no neck remnants (RROC 2). Three patients had residual aneurysm filling (9% RROC 3). Follow up demonstrated complete aneurysmal occlusion in 31 patients (94% RROC 1). One residual aneurysm was completely occluded on follow up (RROC 1). Two patients showed stable residual aneurysmal filling (RROC 3) without clinical significance,” the authors report.
Further, in the subgroup of the 11 wide-necked aneurysms treated using the kissing-Y technique, one basilar artery/superior cerebellar artery aneurysm was treated by sole stenting because the superior cerebellar artery rose out of the aneurysmal fundus. Seventeen months’ follow-up showed stable aneurysm size. In the aneurysms treated by stent-assisted coiling with the kissing-Y technique nine of 10 showed immediately complete occlusion (90% RROC 1).
Brassel et al conclude that their study demonstrates that the use of Acclino stents for stent-assisted endovascular techniques of complex intracranial aneurysms leads to a very high mid-term occlusion rate. As for how the Acclino stents measure up to similar devices for the treatment of intracranial aneurysms, Brassel et al discuss the recent reports of the Leo Baby stent (Balt) and the LVIS stent (Microvention).
“Aydin et al [AJNR Am J Neuroradiol. 2015;36:1934–41.] recently reported an immediate occlusion rate for Leo Baby stents of 75% and 85% on follow up. The immediate occlusion rate using LVIS Jr stents was 73% in a prospective study [Neuroradiology. 2014;56:389–95.] published in 2014. Poncyljusz et al [J Neurointerv Surg. 2015;7:524–9.] reported a RROC 1 of 82% in their LVIS series. Similar results were published by Fiorella et al [J Neurointerv Surg. 2016;8:894–7.] with a complete occlusion rate of 75%. In our study, stent-assisted coil embolisation of wide-necked intracranial aneurysms using the Acclino stents showed a complete occlusion rate of 94%,” they report.













