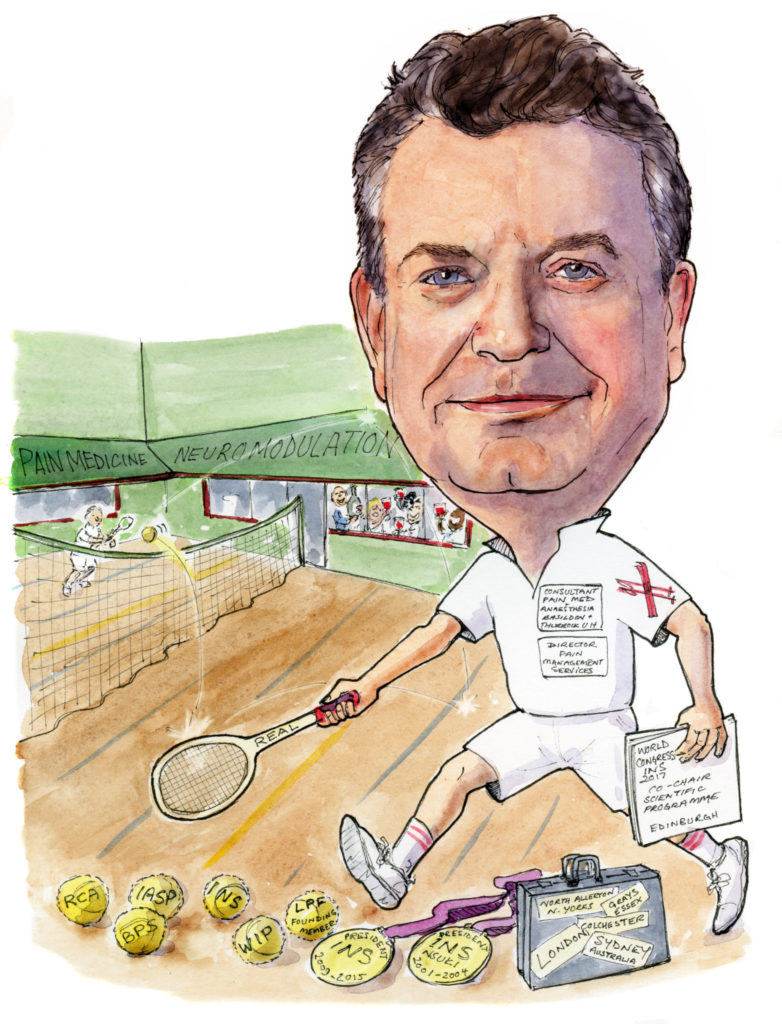
 With a history of medicine in his blood and almost 30 years in the pain management field, Simon Thomson has been at the centre of the development of the field of neuromodulation. A past president of the International Neuromodulation Society (INS) and the founding president of the Neuromodulation Society of the United Kingdom and Ireland (NSUKI) he has played an important role in its evolution. Here he speaks to NeuroNews about how he has seen the field change and grow, his hopes for the future and his interests outside of medicine.
With a history of medicine in his blood and almost 30 years in the pain management field, Simon Thomson has been at the centre of the development of the field of neuromodulation. A past president of the International Neuromodulation Society (INS) and the founding president of the Neuromodulation Society of the United Kingdom and Ireland (NSUKI) he has played an important role in its evolution. Here he speaks to NeuroNews about how he has seen the field change and grow, his hopes for the future and his interests outside of medicine.
What drew you to medicine and to pain medicine and neuromodulation in particular?
I come from a dynasty of medical practitioners. My grandfather was an early radiologist and my father a general practitioner (GP). The world of a GP was very much linked to family life so I was immersed in this world whilst I was growing up. I became aware of pain medicine as a trainee in anaesthesia. I realised that I was not getting any training. I had wanted to live and work for part of my training in Sydney, Australia so in 1989 I took a clinical fellow position at the Royal Prince Alfred Hospital and met Dr John Ditton. John ran a multidisciplinary chronic pain service and was an early pioneer of spinal cord stimulation (SCS) in Australia. I was hooked on both pain medicine and neuromodulation from that moment.
On return to UK, I completed my training, during which I trained with Dr Beverley Collett, a leader in multidisciplinary pain medicine within the UK.
In 1992, at the age of 32, I was appointed a consultant in anaesthesia with special interest in pain medicine at Basildon & Thurrock University Hospitals. There was no established pain medicine there, so I had to build it from scratch. Twenty five years later I continue to lead a good multidisciplinary service and clinical research team.
You have been practising for a number of years. How have you seen the field of neuromodulation change and develop over that time?
Neuromodulation is a fast evolving field. Technology of the devices has improved, in line with technology advances more generally. The clinical science tends to lag behind the technological developments. Sometimes one wonders if the tail is wagging the dog. This is typical of device development. I am proud to have contributed to several of the pivotal studies, regulatory and reimbursement processes that have established SCS as a core treatment in today’s medicine.
I welcome the genuine competition in our SCS field, however, we all have to be aware, like with all product claims that marketing messages may not always reflect the real-world use.
Turning to the technology, there have been several developments that have improved safety and efficacy. The gradual switch of our professional groups from open paddle lead insertion to through the needle insertion is welcome as there are now few real advantages of a paddle lead as a primary procedure. This reduces the occasional incidence of neurological harm, promotes day case ambulatory hospital stays and makes the therapy more accessible. Robust lead design and mechanical anchors have dramatically reduced lead revision procedures. Sixteen contact lead arrays is now the normal (when I first started we just had a 4 contact single lead). Rechargeable devices allow higher energy demand for use with multiple site targeting and high energy for higher frequency programming. In well-selected patients a rechargeable device is cost effective too. Feedback systems to allow real-time optimisation of the stimulation may offer advantages. New targets such as the dorsal root ganglion or intra-epidural nerve roots offer some advantages too.
There is a renewed interest in trying to understand some of the mechanisms of action of neurostimulation in pain, ischaemia and visceral pain.
In your opinion, what has been the most practice-changing advance in terms of treatment options and devices?
The most practice changing development is still a work in progress. There are compelling arguments to change from a wide patient selection, prolonged trial and implant practice to a focussed patient selection, on table trial and implant practice. This does not have to be your whole practice, but in my case it would likely be 90% of my practice. This would mean a major change for countries like the USA. There are many hurdles, but patients, in my experience, when given the choice mostly prefer the single-stage procedure.
Selection, surgical expertise, follow-up and choice of technology are the four pillars of success.
What has been the biggest disappointment—i.e. something that you thought would be practice-changing but was not?
Implantable pulse generator (IPG) and anchor site pain is still a problem in 20% of patients. It can require revision or explantation in up to 5% of patients. We don’t see it much with pump implants, even the non-analgesic ones with baclofen. Is it size? I don’t think so. Is it patient related? Possibly. The hope is that a tiny IPG within the lead tail or attached will improve on this. It remains to be seen.
What is on your wish list in terms of the future development of neuromodulation therapy?
There is no doubt that technology is getting cleverer. We already have closed loop devices and more will likely follow. I think artificial intelligence will become commonplace. We need to take out cost both clinical and device and expand our indications. I believe we need more investment in high-quality clinical research. We cannot rely on intellectual property rights to drive this. We have to find a way to finance clinical research in our field for the good of humanity, not just shareholders.
Do you believe that neuromodulation should be the standard of care for the treatment of chronic pain? How can this become a reality?
Yes, of course I do. I think without question it should be so for chronic neuropathic pain. Neuropathic pain is associated with severe deficits of health-related quality of life and responds poorly to opioids. Neuromodulation must be positioned ahead of opioids. To do that it has to be much more accessible with shorter times from diagnosis of refractory pain to neuromodulation.
You are the chief investigator of the PROCO trial which has recently shown no significant difference in pain relief between 1kHz and 10kHz SCS. What are the potential implications of these results on current practice?
I have been involved with clinical research in the field of pain management and neurostimulation since I started as a consultant, but in recent years this has become a greater part of my working life. The PROCO study was designed to answer a specific clinical question. Through clever study design, collaborative effort and steadfast volunteer patients we were able to provide an answer on which we can rely.
I think the PROCO study will be a good example of study design for the future. When it is possible to double blind and limit bias we should take steps to achieve that.
The results show that there was no significant difference in clinical outcome of chronic neuropathic back and leg pain patients between the selected kHz frequencies having used a carefully selected bipole and optimisation of amplitude and pulse width at each kHz frequency.
This study brings some research clarity to the sometimes frenetic market place of sub-perception SCS. It will be helpful to patients and clinicians.

In your opinion, is there still a need for high frequency stimulation for chronic pain?
Yes, remember that the PROCO study showed that there was a >50% pain reduction from baseline with whatever kHz frequency was used. They are all high frequency. So PROCO is a thumbs up to kHz frequency SCS, its just that we don’t have to be dogmatic, we just have to optimise.
What are your other current research interests?
Currently I am interested in improving the clinical pathway for implementation of SCS. I am collaborating with a National Institute of Healthcare Research project that looks at the value of a prolonged trial phase of SCS versus a short on table trial of SCS and immediate implantation. I am also involved in a search for biomarkers for SCS outcome. Finally, after 10 years I am hopeful that the NSUKI National Neuromodulation Registry will go live in 2017.
What was your most memorable case and what did you learn from it?
I call this case “The Miracle of Orsett”! A 40-year-old paraplegic mother who had had a complete spinal cord injury 20 years prior. She had severe dysaesthesia and allodynia at left L1 distribution. She had moderate neurogenic pain in both legs as well. She had had spinal reconstruction at L1 but had a severely kyphoscoliotic spine. I chose to offer SCS to treat the L1 pain (as this can be helped by SCS) and it was her main problem.
I also had a live surgery-training event with 40 colleagues watching me via video link. It took an hour before I got a single 16 contact lead into the midline of epidural space.
During on-table testing it became apparent that we were able to evoke stimulation not only in the thigh but throughout her whole trunk and lower limbs. The patient started to weep, so did I (but I do weep in movies too!) and so did the audience. It was a wonderful learning experience in so many ways. Three and a half years later she still has no pain; although she hasn’t started to walk though!
Who were your mentors and what impact have they had on your career?
My early mentors were Dr John Ditton in Sydney and Dr Beverley Collett in London then Leicester. However my neuromodulation mentors have been many. I think Elliot Krames must be mentioned. Not only has he been inspirational in the field but he also showed me how his and my brand of leadership, (just getting on with things no matter where you are in the medical hierarchy) can be done successfully.
I have met many wonderful colleagues. One I would like to mention as he probably few realise the influence he has had behind the scenes. In 2001 onwards I worked with Professor Rod Taylor a statistician and trial designer. At that time, he helped bring just enough order to our collective evidence base to convince payers to make SCS a treatment that is a standard of care.
I am lucky enough to count as my friends many of the pioneers and leaders in our field. There are so many connected with the International Neuromodulation Society, past and present to whom I owe much thanks. If I start to list them, I will only miss some out!
What advice do you hope your mentees and students will always follow?
I have been lucky enough to have had five clinical fellows. One I work with as a colleague; the others now work at prestigious University Hospitals in London and Oxford. I hope to have more but there are too few eligible post pain-training fellows.
My main advice is to remain patient-centred, use a limited range of techniques drawn from pharmacology, psychological practice, physical therapy, interventional pain medicine and neuromodulation. One size does not fit all, but nor does random treatment selection. So find the balance. I also believe that one should recognise early when one mode of therapy is not likely to be successful. Challenge all dogmas. Sometimes established theories need to change. When they do it seems obvious in retrospect.
What are your interests/hobbies outside of medicine?
I am an enthusiastic gregarious person. I have had such fun raising my three fine children (all in their twenties now) and have enjoyed travel and sports. I like to play tennis (Real tennis), sail (fairweather), ski (bright skies), blue-sky think and entertain. I am not a singer nor musician but I am a good cook and oenophile.
Fact file
Current position
Consultant in Pain Medicine and Neuromodulation and director of Pain Management Services at Basildon and Thurrock University Hospitals NHS Foundations Trust, Basildon, UK
Education
1973–1978 Radley College, Oxfordshire
1978–1983 Middlesex Hospital Medical School
Qualifications
1980 Certificate of Merit in Biochemistry
1983 MBBS (London)
1988 FRCA January
2002 FIPP
2008 FFPMRCA
Special interests
- Implantable neuromodulation devices for chronic pain and spasticity
- Interventional pain management
- Multidisciplinary pain management
- Refractory angina management service
- Education in pain management for primary and secondary care
Research projects (current)
- National Neuromodulation Database – Inception, Design and Implementation – Principal investigator
- RELIEF Study – Multicentre Observational three year outcome after spinal cord stimulation – Chief investigator
- PROCO – Evaluation of Stimulation Pulse Rate on Clinical Outcomes in Patients whose Pain is controlled by 10KHz Frequency – Chief investigator
- Pilot feasibility randomised comparison trial of facet joint steroid injections versus sham in low back pain
- Multifidus nerve stimulation for chronic low back pain – Mainstay Reactiv8 PMCF study
- TTorNTT – RCT of trial versus no trial strategy for spinal cord stimulation
Society memberships
- Royal College of Anaesthetists
- British Pain Society
- International Association for the Study of Pain
- International Neuromodulation Society
- World Institute of Pain
- London Pain Forum – Founding member













I was a patient of Simon’s from around 2007 till now – He offered me a spinal implant when all else had failed, it changed my life. He went into battle with my Insurers for funding as they were very reluctant to spend a lot of money on a treatment that was in its infancy. Thank you Simon