In response to a growing body of evidence of the existence of “covert” brain injury to patients undergoing transcatheter aortic valve implantation (TAVI) and other cardiac procedures, The Neurologic Academic Research Consortium (NeuroARC) has announced the simultaneous publication of a consensus paper offering a new classification of neurologic outcomes and testing to better ensure the safety of cardiac procedures. The paper is available online, and will be published in the Journal of American College of Cardiology and a future issue of the European Heart Journal.
“As even the smallest damage to particular parts of the brain can impact a patient’s memory and day-to-day ability to function, my colleagues and I have grown increasingly concerned that safety evaluations of the newer cardiovascular procedures only evaluate the extreme life-threatening forms of brain damage,” says Alexandra Lansky, professor of Medicine, Yale University School of Medicine, lead author and co-chair of The NeuroARC. “This paper outlines the need to use and report more modern and sensitive measures to evaluate brain injury related to cardiac procedures.”
The consensus paper is the product of collaboration among leading physician/scientist experts from academic research institutions in the USA and Europe as well as regulators from the US Food and Drug Administration, and representatives from the medical device industry.
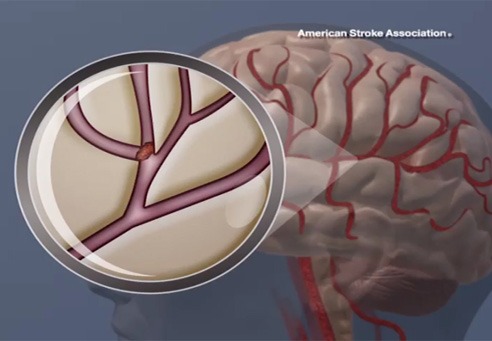
The paper highlights that strokes are among the most feared and costly complications of cardiovascular interventions, and are under-reported in clinical trials. It raises the important point that even minor damage to the brain that has been observed in patients undergoing cardiac procedures can affect the patient’s processing speed and executive function as well as fundamental functions such memory, language, and balance.
“Until now, many studies evaluating the safety of TAVI and other cardiovascular procedures only recorded the most devastating strokes, which meant that doctors—and their patients—were unaware of the full risk potential,” says Michael Mack, co-chair, NeuroARC and chair, Cardiovascular Governance Council, and medical director, Cardiovascular Surgery, Baylor Scott & White Health, Dallas, USA. “We hope this paper will cause researchers to report their findings in a more comprehensive and consistent way so that clinicians can properly interpret the results to provide the best care to patients.”
The paper offers a simple classification of the levels of potential damage to the brain in an effort to allow for better consistency and comprehensive reporting of results
- Type 1: Overt damage to the central nervous system represents neurologic damage with symptoms of stroke, such as weakness or paralysis
- Type 2: Covert injury to the central nervous system represents neurologic damage without apparent symptoms of stroke, but recognized by brain imaging
- Type 3: Neurologic dysfunction without detectable injury, including transient neurological symptoms such as temporary weakness, numbness, slurred speech or delirium without any evidence of damage on brain imaging
“A unique aspect of the consensus is that it identifies three different categories of trials and adapts recommendations for assessments and endpoints as appropriate for the procedure,” says Andreas Baumbach, professor of Medicine, St Bartholomew’s Hospital and Queen Mary University of London, London, UK, and co-chair of NeuroARC. “By tailoring neurologic assessments to the goals of the procedure we hope to be able to demonstrate the benefit of protecting the brain during cardiac procedures.”
“In order to properly assess the impact of various cardiovascular procedures, we recommend specific standardised and validated methods of evaluation,” says Steven Messé, associate professor of Neurology, in the Perelman School of Medicine at the University of Pennsylvania and Co-chair of NeuroARC. “We hope the adoption of these recommendations will improve our ability to evaluate the risks of cardiovascular procedures and the safety and effectiveness of preventive therapies.”











