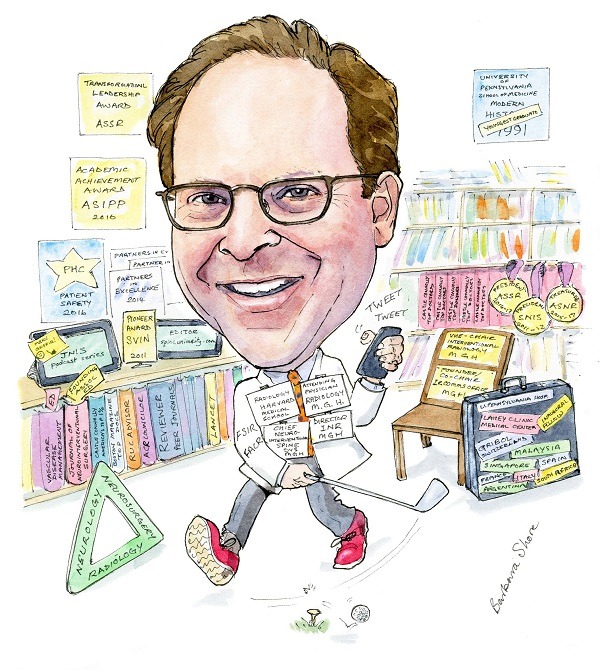
 At just 21-years-old, Joshua A Hirsch was the youngest person in modern history to graduate from his medical school. Since then, he has enjoyed an exciting career with a wide range of interests. He tells NeuroNews about the growth that he has observed in the neurointerventional field and his involvement in its development, his thoughts on healthcare reform in the USA and his interests outside of medicine.
At just 21-years-old, Joshua A Hirsch was the youngest person in modern history to graduate from his medical school. Since then, he has enjoyed an exciting career with a wide range of interests. He tells NeuroNews about the growth that he has observed in the neurointerventional field and his involvement in its development, his thoughts on healthcare reform in the USA and his interests outside of medicine.
What drew you to medicine and to interventional neuroradiology in particular?
As a young man, I was on a trip with my family and we were introduced to a surgeon who described work that was remarkably impactful on people’s lives. It made a huge impression on me and from that time forward, I knew that I wanted to be a physician. That early focus led to an unusual educational pathway. Medical school was enchanting and I found myself excited over and over again by so many different disciplines. Back then, neurointerventional was a nascent field, but focused on improving the lives of patients with cerebrovascular disease. To me, these minimally invasive approaches appeared to be the future. For example, the simplicity of opening a blocked blood vessel and “curing” a stroke held tremendous appeal. My application for radiology residency included specific reference to my then already formed plan of ultimately becoming a neurointerventionalist.
We noticed that you graduated medical school at the age of 21. How did it feel to be so young with so many responsibilities?
It is true that at one point I was a young man. I think it is fair to say that I am taking care of that problem with every passing day. Circumstances came together such that I finished college and hence medical school unusually early; this was not by design. When I was younger, e.g., deciding to go to college, I had some apprehensions about social circumstances that might be uncomfortable for a teenager. This turned out to be unwarranted as I had a wonderful time in both college and medical school. Graduating early allowed me to jump-start my education into a field that at the time required two fellowships. Beyond that, neurointerventional was (and is) a field that benefits from vigour and imagination; both of which are gifts that are not necessarily appreciated by but bestowed upon the young. All in all, I consider myself very lucky to have had this jump-start.
Who have been your career mentors and what have you learned from them? How does that mentorship impact you today?
Mentorship is something I believe in at my core. As a diagnostic neuroradiology fellow, I worked with Dr Bob Grossman; a brilliant man who built an incredibly powerful division. His love of scholarship is the stuff of legends and inspires me even now to make scientific contributions. Dr In Sup Choi taught me how to be a neurointerventional specialist; his knowledge and skill set were phenomenal. I aim to always pass this gift forward and currently derive great pleasure from mentoring others in multiple roles now.
You played an important role in the development of interventional neuroradiology and its training programme at Massachusetts General Hospital. Can you tell us about that?
Massachusetts General Hospital (MGH) has a storied tradition of neurointerventional care—it was one of the first programmes in the USA. The situation was a bit challenging back in 2003 when I was recruited there as personnel changes had left the division very short staffed. Over the following five to six years, attention to clinical excellence and a systematic can-do attitude allowed our group to experience remarkable growth in neurovascular. Beyond that, we established and developed the division’s spine practice. As with all successful efforts we focused on team building and quality improvement. For instance, our group established a unique case quality programme where neuroradiologists, neurologists and neurosurgeons all contributed to robust quality efforts designed at educating and improving our practice—this was really something special, we could do a whole interview about that. Simultaneous with our clinical and operational growth, the division’s academic productivity and service to organised medicine turned up several notches with well over 100 papers being published by members of our group over the next several years. The key, in my opinion, was to focus on clinical excellence—that results in a strong foundation that makes all the other elements possible.
Throughout your career you have promoted the idea of a “multidisciplinary framework for optimised practice”—what does this entail and why is it important?
This is an area where my belief system can get ahead of reality. I am a firm believer in organising practices around centres rather than along traditional departmental lines. Such a framework facilitates triage across a particular pathology. There are three sides of the neurointerventional triangle; neuroradiology, neurology and neurosurgery, and of course many other contributing services. When I joined MGH, we had a staff neurosurgeon working with then two neuroradiologists in neurointerventional. Prioritising our multidisciplinary approach alongside training excellence, we admitted a gifted vascular neurologist to our fellowship. In collaboration with my neurointerventional partners and with the strong support of Dr Jim Thrall, then chair of Radiology, we hired this neurologist when he finished his training making ours, to my knowledge, the first programme in the world to include staff members from all three components of the neurovascular triad as staff. Our staff composition and trainees reflected this deeply held belief that a multidisciplinary framework is best in neurointerventional care, and this triad of multidisciplinary expertise remains as the structure today.
Outside of clinical practice you have an obvious interest in service to organised medicine. Beyond that, you are a prolific author and editor. What spurred these interests in you?
Service writ large is something that my siblings and I learned the value of from a very young age. In terms of professional service, it has always struck me that our opportunity to contribute can occur at many levels. At its most basic (and most satisfying) level, helping a single patient is incredibly rewarding. That “one patient at a time” approach drives me. Separately, I have had the privilege of being elected by my peers to the Boards of five professional organisations serving a range of constituent physicians. These positions facilitate translating that extraordinary feeling of helping a single patient to a shared sense of being able to help people around the world by enabling and supporting their physicians, as well as impacting on broader issues affecting us collectively, such as economic and government issues facing academic radiology, and development of national stroke treatment quality metrics. I do believe this type of service can elevate professional satisfaction while having a meaningful impact on others beyond your own practice. Physicians are the best advocates for themselves and the patients they serve.
In terms of writing, I think that mostly reflects having a relatively poor social life. In reality, I am excited to share advances whether they are clinical, operational or relate to healthcare policy. Being excited about such a broad range of topics lends itself to wonderful publication opportunities. Finally, one of the great joys of my non-clinical professional career has been to serve as an associate editor of the Journal of NeuroInterventional Surgery (JNIS) since its founding. The evolution of the journal has been fantastic and it feels amazing to have been a part of it all this time.
Which innovations in neuroradiology have shaped your career?
There are so many. All neurointerventional specialists have been impacted by famous efforts like those of Guido Guglielmi at UCLA but this question personalises it. Perhaps the unique chain of events that led Lee Jensen and Jacques Dion to place PMMA in a vertebral body in the mid 1990s, which over the following two decades alleviated so much suffering in vulnerable patients worldwide. Perhaps the realisation that using a stent retriever could improve outcomes after stroke treatment or that improving long understood straightforward options like aspiration for stroke treatment could be game-changing. All of these innovations have had dramatic impact on alleviating suffering and improving numerous patients’ lives. They have thus shaped my career.
What is something you thought would be practice-changing but was not, and where is there room for improvement in current practice?
There is a complexity hiding in this straightforward question. One example relates to identifying patients who will benefit from neurointerventional treatment of stroke. Over the last decade, our group has focused on the concept that patients with a significant neurological deficit, blocked blood vessel, and small infarct at presentation, benefit from reperfusion treatment. Our paradigm informed some of the recent landmark stroke trials, and continues to be replicated in high-volume academic stroke centres worldwide. There is always room for improvement—perhaps we could be alleviating suffering in more stroke patients by extending our clinical paradigm beyond the six-hour timeframe suggested by existing guidelines.

Current practice is also being adversely impacted by the commercially available electronic health record (EHR) systems that support care. The reasons for the widespread adoption of primitive systems are pretty straightforward in my mind but beyond the scope of our conversation. Physicians, including neurointerventional specialists, neurologists and many other practitioners spend copious time dealing with the administrative requirements of using these EHR systems. Moreover, they have at times taken humanistic elements out of the physician-patient relationship and this is a shame.
Finally, having witnessed trials in both the neuroendovascular space and minimally invasive spine space get reported as negative and seeing learning opportunities erode, and confusion in the literature amongst physicians, policy experts and payers that impacts on patients, it is my hope that trials are used as learning opportunities to improve practice (as occurred with stroke). In this era of uptodate.com, Wikipedia, technology assessments, there is a real danger that on the basis of limited “negative” data, patients could be denied access to clinically meaningful treatment.
Much of your more recent research and writings have been centred on healthcare economics and policy—why is this area so interesting to you?
While I was always somewhat interested, being elected president of the Society of Neurointerventional Surgery (SNIS) really motivated me to learn more about healthcare policy and economics. My thought was that neurointerventionalists needed to empower themselves to address the challenges that were on the horizon. That plan to educate myself so as to help inform my colleagues expanded beyond neurointerventional as that type of approach was appreciated by my diagnostic radiology and neuroradiology colleagues. I continue to believe that physicians are and need to be the strongest advocates for their patients and that engagement in these types of issues is our best approach to optimising care.
What is your hope for the future of healthcare reform in the USA in light of the current political climate?
I think they used to call that the $64,000 question! Where to begin? Fee for service is felt by many of those involved in healthcare policy to be at the heart of America’s healthcare problem. The authors of the Affordable Care Act (ACA) would argue that it was an effort to augment our existing framework of healthcare insurance. Without question, people at the lower end of the income spectrum have benefited from many of its programmes. Unfortunately, there have been legitimate challenges for middle-income people impacted by high out-of-pocket expenses. The Republicans argued to “repeal and replace” the ACA for multiple election cycles and it would appear that such arguments catalysed their success at the ballot box. Now, the Republicans have what could be termed a problem; rhetoric needs to be turned into policy. The challenge is that given the current political climate, they will likely need to do it on their own—a critique Republicans had visited on the Democrats. One thing that is clear, slowly but surely the system is focusing on value over volume. I believe that neuroendovascular and radiology, on the whole, can and should succeed in that model, but it will require a different focus on how care is often currently provided.
What do you think is the value of social media tools like Twitter in the medical field?
As a Board Member of SNIS, I joined various social media outlets in order to support our engagement efforts around younger members. Having joined Twitter, I paid almost no attention to my account for many years. I became active at a SNIS meeting approximately 18 months ago and never really looked back. I absolutely love the way Twitter quite naturally and efficiently curates information of interest to me and the ability to share various policy, scholarly or other thoughts (in 140 characters or less). In my opinion, every resident and fellow should become active on Twitter. There are many reasons for do so, but, the accelerated way it would allow young people to “get their names out” is truly amazing.
What advice do you hope your mentees will always follow?
Put the patient first, always.
What are your interests outside of medicine?
I love spending time with my incredibly dynamic and supportive family. Live music almost independent of the genre is great; I particularly like classical music and jazz. Reading non-fiction historical accounts has been a joy really since I was a kid—this contributed to my college experience of having a non-scientific major and minor. I am an avid sports fan and over time this has resulted in a migration to all Boston based teams (sorry Dad). Sadly, my fondness for sports does not derive from personal talent; I enjoy testing my jump shot, hitting a baseball or landing one on the green but remain pretty confident that I will always remain an amateur. Finally, while I don’t do this nearly often enough, I very much enjoy exploring new places and whenever possible immersing myself in the local culture.
Fact File
Current position
Vice Chair of Interventional Radiology, Service Line Chief IR, Director Interventional Neuroradiology, Chief NeuroInterventional Spine, Massachusetts General Hospital, Boston, USA and Harvard Medical School, Boston, USA
Education
- 1987 BA Valedictorian, summa cum laude, Touro College, New York, USA
- 1991 MD Alpha Omega Alpha, Piccun Prize University of Pennsylvania School of Medicine, Pennsylvania, USA
Postdoctoral training
- 1991–1992 Intern, Medicine, Pennsylvania Hospital, Pennsylvania, USA
- 1992–1996 Resident, Radiology, Hospital of the University of Pennsylvania, Pennsylvania, USA
- 1994–1995 Fellow, Neuroradiology, Hospital of the University of Pennsylvania, Pennsylvania, USA
- 1996–1997 Chief Fellow, Neuroradiology, Hospital of the University of Pennsylvania, Pennsylvania, USA
- 1997–1998 Fellow, Interventional Neuroradiology, Lahey Clinic Medical Center, Burlington, USA
Service to Organized Medicine (selected)
- 2007- Board Member American Society of Interventional Pain Physicians Kentucky, USA
- 2011–2012 President Society of NeuroInterventional Surgery Virginia, USA
- 2011- Advisor Specialty Society Relative Value Scale Update Committee American Medical Association Illinois, USA
- 2015–2017 Treasurer American Society of Neuroradiology Illinois, USA
- 2016–2017 President American Society of Spine Radiology Illinois, USA
Honours and awards (selected)
- 2006 Named Fellow of Society of Interventional Radiology
- 2010 Named Fellow of American College of Radiology
- 2011 Pioneer Award Society of Vascular and Interventional Neurology
- 2016 ASIPP Academic Achievement Award
- 2017 ASSR Transformation Leadership Award
- 2017 ASNR Distinguished Service Award









