One New York City-based centre is projecting that door-to-puncture times for the endovascular treatment of acute ischaemic stroke patients can be reduced to as low as 15 minutes with the introduction of a new stroke emergency centre featuring the Miyabi imaging system (Siemens).
At the Society of NeuroInterventional Surgery Annual Meeting (SNIS; 24–27 July, Colorado Springs, USA) Reade De Leacy (Mount Sinai Health System, New York, USA) reported his centre’s efforts to reduce time to reperfusion in the endovascular treatment of acute stroke patients.
Previous trials demonstrate a link between the time to reperfusion and patient outcomes. “When we look at the life cycle of a stroke patient, between when they present with their first symptoms and when they are revascularised, we may break it down into two segments—the procedural time, which has become very short, versus stroke systems, and stroke systems are where we can take a lot of time off from when patients present to when they are revascularised and hopefully end up with better outcomes,” De Leacy explained.
Looking specifically at reperfusion times after CT, data from the SWIFT PRIME trial showed that as patients get further out from their initial CT scan to reperfusion, the likelihood of a good outcome significantly drops beyond two hours and the curve starts to dip after 20–30 minutes.
In response, Mount Sinai is setting up a dedicated stroke emergency centre, which is intended to be the first modern stroke emergency centre design in the neurothrombectomy for stroke era that would maximise the quality as well as the timeliness of reperfusion.
“Our goal is to shorten time as much as possible,” De Leacy said.
The proposed stroke emergency centre will have a street level entrance for patients immediately presenting with stroke symptoms. As soon as the patient enters the “stroke ED”, still on the ambulance stretcher they proceed directly to the hybrid suite, which is situated at the end of a small physical space minimising the considerable time wasted with patient movement from the emergency room, to radiology and finally the angiography suite and eliminating all but one patient transfer.
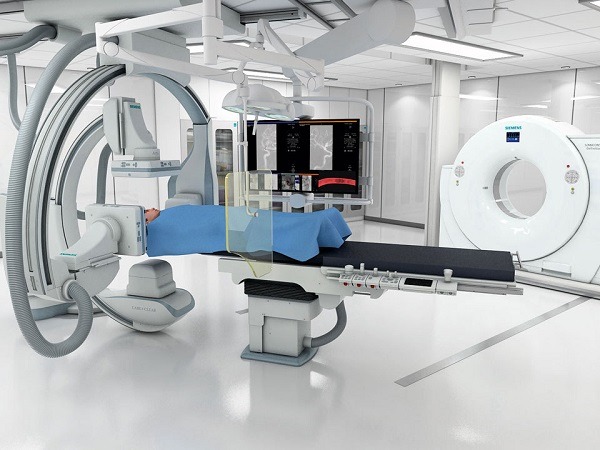
According to De Leacy, the new Mount Sinai Queens stroke emergency centre will be less than 4,000 sq ft, with direct patient pathways from the street to the hybrid CT/Angiography suite. The CT and angiography table are one and the same. Following the CT, the table is rotated from its CT positioning to the angiography configuration. While this is occurring, the neurointerventionalist can review the imaging and the stroke team prepare the interventional devices and lines eliminating unnecessary patient movement and transfers and streamlining the entire process.

The Miyabi system is an Artis Q biplane with a two-room solution. “The two-room solution is very important to maximise the space and the utilisation of the system. For us, the two-room solution was absolutely critical—there is not a lot of space, and this way we can have a system where patients could be triaged during their stroke, get their scan and go straight around to have their angiograms performed and be treated at the same time. We have the CT scanner with a partition that is removable in the middle of the hybrid room,” he explained.
The versatility of the Miyabi system is uniquely suited to a stroke ED setup. The system maximises the use of a small physical space and has the potential to eliminate significant time waste spent transporting and transferring patients to their final destination, permitting the necessary steps involved in emergent large vessel occlusion (ELVO) treatment to be carried out in a streamlined parallel fashion. A room that can be partitioned also allows the CT and angiography systems to be used independently for other purposes such as overflow cross sectional imaging (emergency, inpatient or outpatient) and elective interventions, respectively.
The current goal in the USA is door-to-puncture times of less than 90 minutes. At Mount Sinai, De Leacy reported, they have been able to get door-to-puncture times down to on average just below 60 minutes.
“But, we think it can be improved. When you look at the timing in systems of care, we think that that is where a lot of time can be trimmed. Optimistically, we think that there is probably 20–60 minutes that we can remove from the current algorithm. So, the aim for door-to-puncture time is less than 90 minutes, at Mount Sinai we are at less than 60 minutes and what we would really want to get to is less than 15 minutes. In order to do this, it cannot be done with just a small footprint emergency department, you have to have an integrated system that is going to cut out the patient transfers,” De Leacy maintained.













