The noninferiority of mechanical thrombectomy alone—compared to mechanical thrombectomy plus intravenous tissue plasminogen activator (IV-tPA)—for the treatment of acute ischaemic stroke has been demonstrated across more than 109,000 patients within a national US database. These results were presented at the International Symposium on Endovascular Therapy (ISET; 9–11 May, Miami, USA).
“Our results indicate that mechanical thrombectomy alone was used more frequently than mechanical thrombectomy plus IV-tPA among patients with acute ischaemic stroke,” Waseem Wahood (Nova Southeastern University, Fort Lauderdale, USA) said. “Both treatment groups had similar odds of mortality, but the mechanical thrombectomy alone group had higher odds of 90-day poor functional outcome compared with the mechanical thrombectomy plus IV-tPA group. These results support the findings in the three recent clinical trials.”
According to Wahood, the results from three clinical trials also investigating the efficacy of various endovascular treatments for patients with acute ischaemic stroke—the DEVT, DIRECT-MT and SKIP studies—were published in 2020 and 2021, with DEVT and DIRECT-MT both demonstrating mechanical thrombectomy’s noninferiority when compared to mechanical thrombectomy plus IV-tPA.
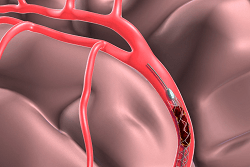
Wahood and colleagues therefore decided to query a national inpatient database, the Healthcare Cost and Utilization Project-National Inpatient Sample (HCUP-NIS), for patients undergoing mechanical thrombectomy for acute ischaemic stroke between 2006 and 2018. Across a total of 109,385 admissions, some 68,940 (62%) patients’ admission involved thrombectomy alone, and the investigators compared these patients to those who underwent thrombectomy plus IV-tPA regarding 90-day poor functional outcome, inpatient mortality rate, and patient profile for tPA usage.
Regarding mortality rate, those who received mechanical thrombectomy alone had “similar odds” of death compared with those receiving thrombectomy plus IV-tPA (odds ratio=1.01; P=0.80). This led Wahood and colleagues to conclude that their own findings were broadly aligned with those of previous trials like DEVT and DIRECT-MT regarding the noninferiority of mechanical thrombectomy alone—in spite of the thrombectomy-alone group seen in their own investigations also having higher odds of poor functional outcome compared with the thrombectomy plus IV-tPA group (odds ratio=1.14; P=0.002).
They found an increase in the trend of mechanical thrombectomy being used without IV-tPA among patients with acute ischaemic stroke (trend=3.27%; P<0.001) over time, with a 72% rate of thrombectomy alone being seen in 2018 compared to just 52% in 2006. Multivariable regression analysis regarding patient profiles indicated that patients who identified as Black (odds ratio=0.83; P<0.001) or Hispanic (odds ratio=0.83; P=0.002) were more likely to undergo mechanical thrombectomy alone compared with those who identified as white.
Additionally, Wahood reported that those in the top quartile of household income had lower odds of undergoing mechanical thrombectomy alone compared with those in the lowest quartile (odds ratio=0.90; P=0.040), while admissions in urban teaching hospitals were more likely to receive thrombectomy alone compared with those in urban nonteaching hospitals (odds ratio=1.61; P<0.001). One key limitation of the study that Wahood also highlighted was the fact he and his colleagues could not control for the time of administration of the different treatment types. “The clinical trials were capped at 4.5–6.5 hours, while the national database we used does not record hour of administration,” he added.










