While the latest thrombectomy techniques, thrombolytic drug candidates and even neuroprotective agents are the source of much discussion in today’s neurovascular space, there is also significant room for improvement within another step along the stroke care pathway: patient triage. For NeuroNews, Jeffrey Saver (Los Angeles, USA) provides a snapshot of the novel technologies being used to improve diagnoses, transfer decisions and, ultimately, patient outcomes.
When a stroke occurs, the prehospital system must respond quickly and intelligently, as treatments are extremely time- and place-dependent. With every nine minutes of delay in the onset of intravenous thrombolysis, one of every 100 patients experiences a more severe disability. As such, it is essential that patients with stroke—or on-scene witnesses—activate the 911 system as soon as possible after onset. Further, when prehospital personnel arrive on the scene, they must distinguish patients with stroke from those with stroke-mimicking conditions and bring the neurovascular patients directly to certified stroke centres capable of providing lytic therapy rapidly.1
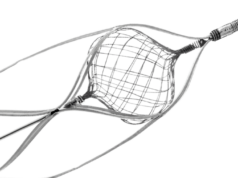
In addition, with every four minutes of delay in the start of endovascular thrombectomy, one of every 100 patients experiences a worse disability outcome. It is therefore desirable that prehospital personnel also distinguish patients with ischaemic strokes due to large vessel occlusion (LVO) from those with small and medium vessel occlusions, and transport the LVO patients directly to advanced stroke centres capable of performing thrombectomy procedures—if not too distant.1
Some patients with intracerebral haemorrhage (ICH) may require immediate ventricular drainage or haematoma evacuation. It is therefore preferable that ICH patients are brought directly to neurosurgical care hospitals, if nearby, though not transported long distances because of their high rate of deterioration before hospital arrival.2,3
Existing solutions
Currently, for these routing decisions, prehospital systems rely on the classic foundation of history and physical exam. Formalised history and examination have enabled implementation of useful regional systems of stroke care but work imperfectly. To detect stroke onset, patients and families are taught the face-arm-speech-time (FAST) mnemonic; but stroke deficits may prevent patients from recognising or acting on symptoms, and the 20% of strokes that occur in sleep are detected only after a delay.
To distinguish strokes from stroke mimics, paramedics use standardised stroke recognition scales, such as the Los Angeles prehospital stroke screen (LAPSS) scale and the Cincinnati prehospital stroke scale (CPSS). However, these only have an accuracy of 60–75%. And, to distinguish LVO from non-LVO stroke, paramedics use standardised stroke severity scales, such as the Los Angeles motor scale (LAMS) or the rapid arterial occlusion evaluation (RACE) scale—but these also only have 60–75% accuracy too. Further, no validated assessment exists to distinguish ICH from ischaemic stroke.
Novel tools and technologies
Fortunately, we stand poised at the threshold of a new era in which mobile health technologies promise to dramatically enhance prehospital diagnostic performance. Immediate detection of stroke onset will occur through wearable and environmental sensor technologies.4 Already, the Apple Watch detects patient falls from stroke and automatically notifies the emergency medical services (EMS) system. Other wearables under development include electroencephalogram (EEG) headbands to monitor for stroke onset during sleep, and bilateral wristbands with accelerometers that monitor for hemiparesis onset in both waking and sleeping patients.
The rise of ubiquitous external video and audio monitoring in modern life provides abundant further opportunities for stroke onset detection technology. Smartphone, video meeting, security and home robot cameras with artificial intelligence visual recognition systems will be able to monitor continuously for onset of facial weakness, limb weakness, or ataxia. Voice assistant, smartphone and home robot audio systems will similarly be able to monitor continuously for the first onset of aphasia or dysarthria. As a result, hyperacute entry into the EMS system will occur for many more patients.
When prehospital personnel respond, their patient assessments will be technologically enhanced. Many biotech companies are currently developing ‘stroke helmet’ technologies that paramedics can place on the patient’s heads to rapidly probe their brain status.5 Alterations in brain physiology by cerebrovascular insults change the brain’s energetic response to these probes in distinctive ways.
Among the wide variety of technologies being developed for paramedic use, some are updates of longstanding neurodiagnostic approaches: ultrasound, EEG, and near infrared. Of particular interest are entirely new approaches including microwaves, electrical impedance and cranial vibrations. All of these technologies have the potential to improve paramedic performance across each of the three key prehospital diagnostic distinctions—stroke versus non-stroke; LVO ischaemic stroke versus non-LVO ischaemic stroke; and haemorrhagic stroke versus ischaemic stroke.
Cautious optimism
One of the innovations with which I am involved, the Harmony device (MindRhythm) that assesses alterations in head pulsation, has advanced to the stage of validation testing in the prehospital setting.6 Others likely will also soon be entering prehospital assessment. We must be wary of overenthusiasm for technological solutions. Many hurdles still need to be overcome before we have a technologically optimised triage system of prehospital stroke care.
But, as Amara’s Law states, while we overestimate the effect of a particular technology in the short run, we underestimate the effect in the long run. I fully expect that mobile health technology will powerfully reshape prehospital stroke care over the next decade.
References:
- Jauch E C, Schwamm L H, Panagos P D, et al. Recommendations for Regional Stroke Destination Plans in Rural, Suburban, and Urban Communities From the Prehospital Stroke System of Care Consensus Conference. Stroke. 2021; 52: e133–e152.
- Shkirkova K, Saver J L, Starkman S, et al. Frequency, Predictors, and Outcomes of Prehospital and Early Postarrival Neurological Deterioration in Acute Stroke: Exploratory Analysis of the FAST-MAG Randomized Clinical Trial. JAMA Neurol. 2018; 75(11): 1364–74.
- Ramos-Pachón A, Rodríguez-Luna D, Martí-Fàbregas J, et al. Effect of Bypassing the Closest Stroke Center in Patients with Intracerebral Hemorrhage: A Secondary Analysis of the RACECAT Randomized Clinical Trial. JAMA Neurol. 2023; 80(10): 1028–36.
- Bat-Erdene B O, Saver J L. Automatic Acute Stroke Symptom Detection and Emergency Medical Systems Alerting by Mobile Health Technologies: A Review. J Stroke Cerebrovasc Dis. 2021; 30(7): 105826.
- Chennareddy S, Kalagara R, Smith C, et al. Portable stroke detection devices: a systematic scoping review of prehospital applications. BMC Emerg Med. 2022; 22(1): 111.
- Smith W S, Paxton J H, Wilburn J M, et al. LBA3 Head Pulse For Ischemic Stroke Detection Prehospital Study During COVID‐19 Pandemic (EPISODE‐PS‐COVID): Initial Trial Results. Stroke Vasc Neurol. 2023; 3(S1): e12451.
Jeffrey Saver works at the University of California Los Angeles (UCLA; Los Angeles, USA), where he is medical director of the Stroke Unit at the UCLA Medical Center, a professor of neurology at the UCLA School of Medicine, and co-director of the UCLA Stroke Center.
DISCLOSURES: The author is a member of MindRhythm’s strategic advisory board.