 With the results of the DAWN trial now published in the New England Journal of Medicine and the late time window data from the ESCAPE trial recently released, the support for a new way of selecting patients for endovascular therapy to treat large vessel occlusion stroke is growing. These results have indicated that, beyond six hours of time last seen well, the determination on which patients are eligible for endovascular treatment should be made using physiological criteria assessed on imaging over the traditional time of stroke onset.
With the results of the DAWN trial now published in the New England Journal of Medicine and the late time window data from the ESCAPE trial recently released, the support for a new way of selecting patients for endovascular therapy to treat large vessel occlusion stroke is growing. These results have indicated that, beyond six hours of time last seen well, the determination on which patients are eligible for endovascular treatment should be made using physiological criteria assessed on imaging over the traditional time of stroke onset.
The DAWN (DWI or CTP Assessment with Clinical Mismatch in the Triage of Wake-Up and Late Presenting Strokes Undergoing Neurointervention with Trevo) trial compared endovascular thrombectomy plus standard medical care with standard medical care alone for the treatment of patients with acute stroke who had last been known to be well six to 24 hours earlier and who had a mismatch between clinical deficit and infarct.
As part of the inclusion criteria in DAWN patients had to have a mismatch between the severity of the clinical deficit and the infarct volume, which was defined according to the following criteria: those in group A were 80 years of age or older, had a score of 10 or higher on the National Institutes of Health Stroke Scale (NIHSS; scores range from 0 to 42, with higher scores indicating a more severe deficit), and had an infarct volume of less than 21ml; those in group B were younger than 80 years of age, had a score of 10 or higher on the NIHSS, and had an infarct volume of less than 31ml; and those in group C were younger than 80 years of age, had a score of 20 or higher on the NIHSS, and had an infarct volume of 31ml to less than 51ml.
Infarct volume was assessed with the use of diffusion-weighted magnetic resonance imaging (MRI) or perfusion CT and was measured with the use of automated software (RAPID, iSchemaView).
Patients were randomly assigned, in a 1:1 ratio, to thrombectomy plus standard medical care (the thrombectomy group) or to standard medical care alone (the control group). The co-primary endpoint was the mean score for disability on the utility-weighted modified Rankin scale at 90 days and the rate of functional independence (defined as a score of 0, 1, or 2 on the modified Rankin scale) at 90 days.
As previously reported in NeuroNews enrolment in the DAWN trial was stopped at 31 months, because the results of a pre-planned interim analysis met the pre-specified criterion for trial discontinuation, which was a predictive probability of superiority of thrombectomy of at least 95% for the first primary endpoint.
One hundred and seven patients were randomised to receive Trevo and 99 patients to receive medical management.
In terms of time-last-seen-well to randomisation, the mean time was 13.4±4.1 (median, 12.2) hours in the treatment arm and 13.0±4.5 (median, 13.2) hours in the control arm (p=0.53), suggesting that more that 50% of the patients were treated beyond 12 hours from time-last-seen-well. In the stroke type sub-population, wake-up strokes were more prevalent in the treatment arm (64.5%) than in the control arm (47.5%), 10.3% of patients in the treatment arm had a witnessed stroke and 25.2% of patients had an unwitnessed stroke, compared with 14.1% witnessed stroke and 38.4% unwitnessed stroke in the control arm.
Core lab adjudicated TICIs post-procedure were as follows: modified TICI ≥2b=84%; original TICI ≥2b=72.6%; and TICI 3=10.4%.
In the weighted mRS based co-primary outcome, the mean mRS value in the treatment group was 5.5 versus 3.4 in the control group; a 2.1 difference in the weighted mRS score, which is highly significant with a Bayesian probability of superiority of >0.9999 (which is equivalent to p˂0.0001). The co-primary endpoint of 90-day functional independence was 49% in the treatment group versus 13% in the control group; a 35.5% actual difference, which is highly significant with a Bayesian probability of superiority of >0.9999. This translates to a number needed to treat of 2.8 to achieve functional independence.
In terms of secondary efficacy endpoints, recanalisation rates at 24 hours were significantly in favour of the treatment group with 77% compared with 36% in the control group (p˂0.001). For all the secondary endpoints, the comparisons between the two treatment groups favoured thrombectomy.
The primary safety endpoint was stroke-related mortality with no significant difference observed between the two groups.
In the New England Journal of Medicine, the DAWN investigators write “Endovascular thrombectomy in patients with stroke is usually performed within six hours after the onset of stroke. However, the rate of functional independence in the thrombectomy group in our trial, in which patients received treatment six to 24 hours after stroke onset, was similar to the rate reported in a pooled analysis of five trials of thrombectomy [HERMES], in which patients predominantly received treatment within six hours after stroke onset (49% and 46%, respectively). In contrast, the rate of functional independence in the control group in our trial was lower than the rate in the control group in the pooled analysis (13% vs. 26%). It is possible that the worse outcomes in our control group were related to the lower rate of treatment with intravenous alteplase (14% in our trial vs. 88% in the pooled analysis); patients were enrolled in our trial after the accepted window of time in which intravenous thrombolytic therapy is typically administered.”
They found that, among patients with acute stroke who have a mismatch between the severity of the clinical deficit and the infarct volume, the safety profile for thrombectomy performed six to 24 hours after the onset of stroke was similar to a previously observed safety profile for thrombectomy performed within six hours after the onset of stroke.
Writing in an accompanying editorial in the New England Journal of Medicine, Werner Hacke (University of Heidelberg, Heidelberg, Germany) emphasises the importance of the DAWN results.
“Some readers may struggle with the Bayesian statistics and unusual primary endpoint that were used in the DAWN trial. They should be assured that the positive outcome of the trial was not due to complex statistical manoeuvring or the use of an unconventional endpoint, which involved a utility-weighted modification of the usual Rankin scale. Even with the use of basic parametric statistics and an endpoint that is typically used in stroke trials, the DAWN trial had strikingly positive results,” writes Hacke.
As for the value of assessing stroke patients for treatment outside of simply the time from onset criteria, Hacke maintains that the DAWN results present a comparable option.
“In the DAWN trial, the rate of the second primary endpoint of functional independence (defined as a score of 0, 1, or 2 on the modified Rankin scale, which ranges from 0 to 6, with higher scores indicating more severe disability) at 90 days was 49%, and in the meta-analysis, the rate was 46%; these similar findings suggest that the use of a ‘tissue window’ in choosing patients for thrombectomy is as good as the use of a time window… These imaging-based approaches represent a new ‘DAWN’ for the selection of patients who are likely to benefit from thrombectomy that is performed far longer after the onset of stroke than current guidelines suggest, at least among patients who have severe stroke, vascular occlusion, and penumbral tissue,” Hacke writes.
ESCAPE late window population
In the ESCAPE (Endovascular Treatment for Small Core and Proximal Occlusion Ischemic Stroke) trial, imaging (CT/CTA) served as a marker of favourable brain physiology instead of time. According to Bijoy Menon et al, in a recent publication in the American Journal of Neuroradiology, this was a pragmatic choice because the patient is often unaware of stroke-onset time or is unable to communicate it clearly.
“Epidemiologic studies suggest that one of every three patients with stroke may either wake up with symptoms or have unwitnessed onset, and this proportion may increase with an ageing population. Patients with unwitnessed stroke onset may have a last-known-well time many hours before or immediately proximate to the time of stroke recognition. Among this group, two types of patients can be identified. Both patients with a true recent infarct onset and patients with good collaterals and slow infarct progression can be identified as ideal therapy candidates. The change to a physiologic paradigm of using time windows to select which populations to screen and then imaging to select those eligible for acute treatment is actively supported by these [ESCAPE late window] results,” the ESCAPE investigators write.
The ESCAPE trial was a prospective, multicentre, randomised, controlled, open-label trial design with blinded outcome assessment. The trial enrolled patients presenting within 12 hours from last seen healthy with disabling ischaemic stroke, a small core infarct on non-contrast head CT (ASPECTS 6–10), and moderate-to-good collaterals on CT angiography.
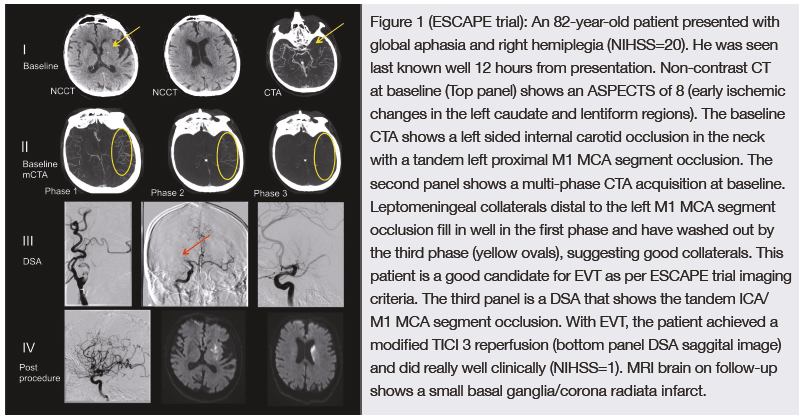
Unlike the DAWN and DEFUSE 3 trials, however, which both used perfusion imaging to select patients for treatment, the ESCAPE trial used head CT and CT angiography (as in Figure 1) as radiographic markers to enrol patients up to 12 hours from symptom onset thus providing a unique perspective on patients presenting to medical attention relatively late.
 Fifty-nine of 315 (19%) patients were randomised >5.5 hours from last seen healthy (at least six hours from stroke onset to puncture). There was no evidence of heterogeneity of treatment effect between the early presenters and patients enrolled in the extended time window (p=0.134, likelihood ratio test).
Fifty-nine of 315 (19%) patients were randomised >5.5 hours from last seen healthy (at least six hours from stroke onset to puncture). There was no evidence of heterogeneity of treatment effect between the early presenters and patients enrolled in the extended time window (p=0.134, likelihood ratio test).
Similar to what was observed in the DAWN trial, a treatment effect favouring intervention was seen across all clinical outcomes in the ESCAPE late window population. In this late window subgroup, intervention was superior to the best medical therapy for NIHSS 0–2 at 90 days (45.5% vs. 13.6%, p=0.019). The absolute risk difference favouring intervention was 19.3% on the mRS 0–2 at 90 days, and the shift analysis (proportional odds model) favoured intervention (adjusted common OR=2.61; 95% CI, 0.9–7.8).
ESCAPE investigator Mayank Goyal (University of Calgary, Calgary, Canada) told NeuroNews that he believes that “from a practical standpoint the imaging criteria used in ESCAPE is much easier to implement and there is a much wider availability of CT and mCTA compared to MR or CTP (and RAPID software).” (Figure 1)
Further, ESCAPE investigator Bijoy Menon (University of Calgary, Calgary, Canada) maintains that “the fact that the ESCAPE trial late window patients who received EVT had very similar outcomes (while not statistically significant) to patients enrolled in the DAWN trial who got EVT while the control arm performed much more in line with expectations does raise the possibility that the simpler and more widely applicable selection criteria of ESCAPE may be sufficient for the late time window as well.”
Upcoming results
We now await the results of the DEFUSE 3 trial—expected to be presented at the International Stroke Conference (ISC; 24–26 January, Los Angeles, USA)—which, following an interim analysis of data from the first 182 patients enrolled, was terminated with a high likelihood of benefit in the endovascular group of the study. With some similarity to DAWN, DEFUSE 3 investigated endovascular treatment in an extended time window of six to 16 hours after stroke onset. Patients who met the inclusion criteria underwent either CT perfusion/CT angiography (CTP/CTA) or magnetic resonance (MR) diffusion weighted imaging/perfusion weighted imaging/angiography (DWI/PWI/MRA) studies prior to randomisation. As in the DAWN trial, these images were processed with an automated image analysis platform (RAPID) to identify patients with salvageable brain tissue (target mismatch profile).
 However, as Werner Hacke cautions in his comment piece, “the results of the DAWN trial do not support a general liberalisation of the time window for thrombectomy or thrombolysis. Reducing the time from the onset of stroke to treatment remains essential and results in the best outcomes. It is likely that a limited proportion of patients with occlusion of a large vessel who present late after the onset of stroke will have a small infarct core and a large volume of tissue at risk, as did the patients in the DAWN trial. For those patients, late thrombectomy works—but as of now, as far as we know, it works only for them.”
However, as Werner Hacke cautions in his comment piece, “the results of the DAWN trial do not support a general liberalisation of the time window for thrombectomy or thrombolysis. Reducing the time from the onset of stroke to treatment remains essential and results in the best outcomes. It is likely that a limited proportion of patients with occlusion of a large vessel who present late after the onset of stroke will have a small infarct core and a large volume of tissue at risk, as did the patients in the DAWN trial. For those patients, late thrombectomy works—but as of now, as far as we know, it works only for them.”









