Late-breaking research presented at the recent Society of NeuroInterventional Surgery’s (SNIS) 19th annual meeting (25–29 July, Toronto, Canada) has shown that thrombectomy procedures can achieve positive outcomes for patients experiencing strokes caused by a basilar artery occlusion (BAO)—despite typically being reserved for the treatment of large vessel occlusion (LVO) stroke.
These findings were delivered by lead author Fawaz Al-Mufti (Westchester Medical Center/New York Medical College, New York, USA), who said: “Patients who receive thrombectomy increase their life expectancy by five years compared to patients who do not. For every 10 minutes saved in getting a thrombectomy, patients experience an additional month of life free from disability. Furthermore, BAO stroke is associated with 40% mortality and, of the survivors, 80% have severe deficits. This is especially true for BAO stroke patients with high NIHSS [National Institutes of Health Stroke Scale], where endovascular thrombectomy portends a mortality and disability benefit.”
Al-Mufti detailed that this research, dubbed the BArONIS study, sought to build on recent breakthroughs achieved in the ATTENTION and BAOCHE studies in China, and assess whether the positive outcomes seen in BAO stroke patients who underwent mechanical thrombectomy procedures in these randomised controlled trials are likely to translate to Western populations.
BArONIS involved conducting a retrospective analysis of the US National Inpatient Sample database and included non-elective admissions of BAO patients with an NIHSS score >9 who received thrombectomy between 2015 and 2019. The study’s primary clinical endpoint was a favourable outcome, measured via ‘routine discharge’ of the patient to their home or acute rehabilitation, while safety endpoints included mortality and symptomatic intracranial haemorrhage.
Across nearly 4,000 patients, this analysis found that BAO stroke patients who underwent thrombectomy were younger, and were more likely to be female, as well as having a slightly higher NIHSS score and rate of atrial fibrillation, on average, than those who did not undergo thrombectomy.
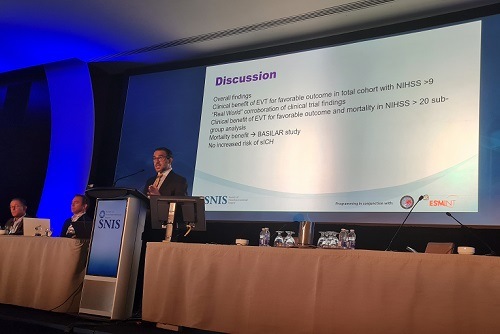
At SNIS 2022, Al-Mufti also detailed that BAO patients treated via thrombectomy were more likely to experience a favourable outcome, and there was no difference in the rates of mortality or symptomatic intracranial haemorrhage between the two groups. In addition, a subgroup analysis revealed that BAO patients with an NIHSS score >20 experienced a statistically significant benefit in terms of mortality rates, as well as favourable outcome benefits, after undergoing thrombectomy.
“We feel that this is a real-world corroboration of the clinical findings demonstrated in both ATTENTION and BAOCHE,” Al-Mufti said. “There are limitations to our study—we lack granularity, and we do not know about time from ‘last known normal’, but hopefully the overall size of the study will dilute the effects of these issues.”
Elsewhere at SNIS, a second study—presented by lead author Ali Alawieh (Emory School of Medicine, Atlanta, USA)—indicated another area that thrombectomy treatments could yet expand into: distal vessel occlusion (DVO) stroke. In this multicentre study, researchers analysed outcomes in nearly 7,500 patients undergoing thrombectomy for different types of strokes across 32 US centres.
They found that, while this is another space in which thrombectomies are not typically deployed, post-thrombectomy clinical outcomes for DVOs were comparable to those seen in patients experiencing LVO stroke. “Thrombectomy has changed the way medical professionals care for patients with stroke,” said Alawieh. “If more stroke patients can experience this lifesaving treatment, we want to ensure that happens.”









