 “It is an amazing time to work in stroke medicine,” Jesse Dawson tells NeuroNews. Looking back at his career, he discusses the field’s biggest disappointment, and, in line with his own interests, believes the future of stroke treatment should embrace the importance of diet and exercise as preventative measures. As co-chair of the joint European Stroke Organisation and World Stroke Organisation Conference (ESO-WSO 2020) Planning Group and Programme Committee, he touches on the themes of the upcoming meeting, with implementing best practices globally and artificial intelligence representing hot topics.
“It is an amazing time to work in stroke medicine,” Jesse Dawson tells NeuroNews. Looking back at his career, he discusses the field’s biggest disappointment, and, in line with his own interests, believes the future of stroke treatment should embrace the importance of diet and exercise as preventative measures. As co-chair of the joint European Stroke Organisation and World Stroke Organisation Conference (ESO-WSO 2020) Planning Group and Programme Committee, he touches on the themes of the upcoming meeting, with implementing best practices globally and artificial intelligence representing hot topics.
What initially attracted you to medicine and stroke therapy in particular?
I have to admit I had no particular desire to be a doctor, it was just what you were encouraged to do when you got good grades at school. However, as soon as I started my studies, it was clear I made the right choice. I was particularly interested in research at a very early stage.
I lack the concentration span to stand for hours in an operating theatre and I find the idea of sticking my hands in someone’s guts rather sickening. So while I have the utmost respect for my surgical colleagues’ skills and abilities, it definitely is not for me.
Cardiology was my favourite subject, but I was not interested in intervention and when I trained it was the boom time for interventional cardiology. I am also five-foot-eight and not remotely macho, so it was not for me either (I am sure it is a bit different now). I liked neurology so stroke medicine was the logical choice. A bit of cardiology and a bit of neurology but unlike “proper” neurology, I would not have to give everyone steroids.
It is an amazing time to work in stroke medicine. Real strides forward are being made and outcomes are getting better and better. My earliest memory of a hospital was seeing my grandmother who had a large stroke whilst visiting us when I was age 10 or 11. I still marvel at how she managed to return home and live independently for years and I think that stimulated my interest in recovery.

Who were your mentors and what impact have they had on your career?
I have been very lucky in the support I have had from a number of people. First and foremost my main mentor has been Professor Kennedy Lees. It is fair to say that my whole career and progress is thanks to his support and guidance. It was a great honour to train under him and an even greater honour to now lead the research group he set up. Although he spends proportionally more of his time at sea now, he is still available for advice and at times when I need it! Another friend and colleague is Professor Matthew Walters, who supervised all my early research projects and is still a great source of support.
More recently I was given the opportunity to join the CLEAR and MISTIE trials by Professor Daniel Hanley, and it was a real privilege to see the diligence and thoroughness with which he conducts his trials. I will measure all my future work on how close I can get to those standards. In the UK we are lucky to have an extremely supportive and thoughtful group of senior physicians and both Professor Gary Ford and Professor Phillip Bath have been sources of support.
In the wake of COVID-19, what impact has the decision to stop scheduling elective procedures had on the work of neurosurgeons, in your experience?
We have not yet seen any changes to neurosurgical work. In our unit, stroke care is classed as acute so it is proceeding fairly normally at the moment. We do expect that to change. We have begun a lot of remote consultations and we are much more circumspect in deciding whether a test or consultation is really necessary.
What positives do you see coming from the COVID-19 pandemic in terms of lessons learnt?
I think these experiments with technology will help streamline our care in the future and we will emerge from this awful episode very deeply wounded, but overall a little stronger.
Throughout your career, what has been the biggest disappointment?
I was very disappointed that the ESUS trials did not demonstrate superiority of anticoagulation over antiplatelets in people with embolic stroke of undetermined source. I thought it made sense and I really did think it would work. However, this serves as an excellent reminder that high-quality trials are always needed to test ideas.
What technology are you currently keeping an eye on?
I think it is going to be fascinating to see how everyday technology such as wearables and phones can be used to predict risk, prevent and detect cardiovascular diseases such as stroke.
I think we will start to see people coming to our clinics in the next few years with their own data on blood pressure, heart rate and rhythm and we will need to act on them.
In terms of preventative treatment for stroke, should the field refine existing treatments or focus their efforts on researching novel approaches?
I am a bit of a fitness fanatic and I am increasingly convinced that we should be focussing on diet and exercise more and more. Sure, we can spend thousands of pounds on new drugs—we all like new stuff and spending money. But if we can find a way to help people move more and eat better, the benefits will be far greater. You do not need to take my word for it, it is all on Netflix. Of course, this will work less well in secondary prevention in people with disability but for primary prevention and in a great many patients, it would be effective.
Could you tell us about the novel treatments for upper limb weakness after stroke that you are working on?
We are currently exploring whether use of vagus nerve stimulation paired with intensive upper limb rehabilitation is effective for improving arm function after stroke. We hope to conclude a phase 3 study in the next year or so. We are also exploring whether use of the Saebo Glove allows people with the most severe arm weakness to better engage with physiotherapy early after stroke.
In your opinion, what are the highlights of the joint ESO-WSO 2020 meeting?
The main highlight of the joint meeting has been in bringing together the ideas from both societies. We have greatly increased the number of presentations giving investigators more chances to present their work. We will have sessions on big data and artificial intelligence as well as sessions on the whole stroke care pathway.
One of our key themes will be on implementing best practices throughout the world. This year we will have more parallel sessions and have had over 3,400 abstracts submitted and over 500 of these will have a form of oral presentation. We have also had presentation of a number of large clinical trials confirmed.
From your research and experience, what motivates you?
I am motivated by trying to find solutions to problems. And also the vanity of seeing one of my ideas make it into clinical practice.
What advice do you hope your PhD and MD students will follow?
Take the initiative. If there is a problem, confront it; find a solution and fix it. Do not just bring a problem to a senior or a colleague. Bring the problem and a suggestion for how to fix it. The suggestion might not be the best solution but that does not matter.
What has been your most memorable case?
I think it was the first time I saw a patient in the stroke unit who was younger than me.
What are your interests outside of medicine?
My family and also, when I am not cycling, all I think about is cycling, and when I am cycling, all I think about is not cycling.
Do you have a fantasy experiment or study?
I would like to see us properly test lifestyle measures in people at risk of stroke; prescribing diets and exercise programmes rather than drugs and surgery.
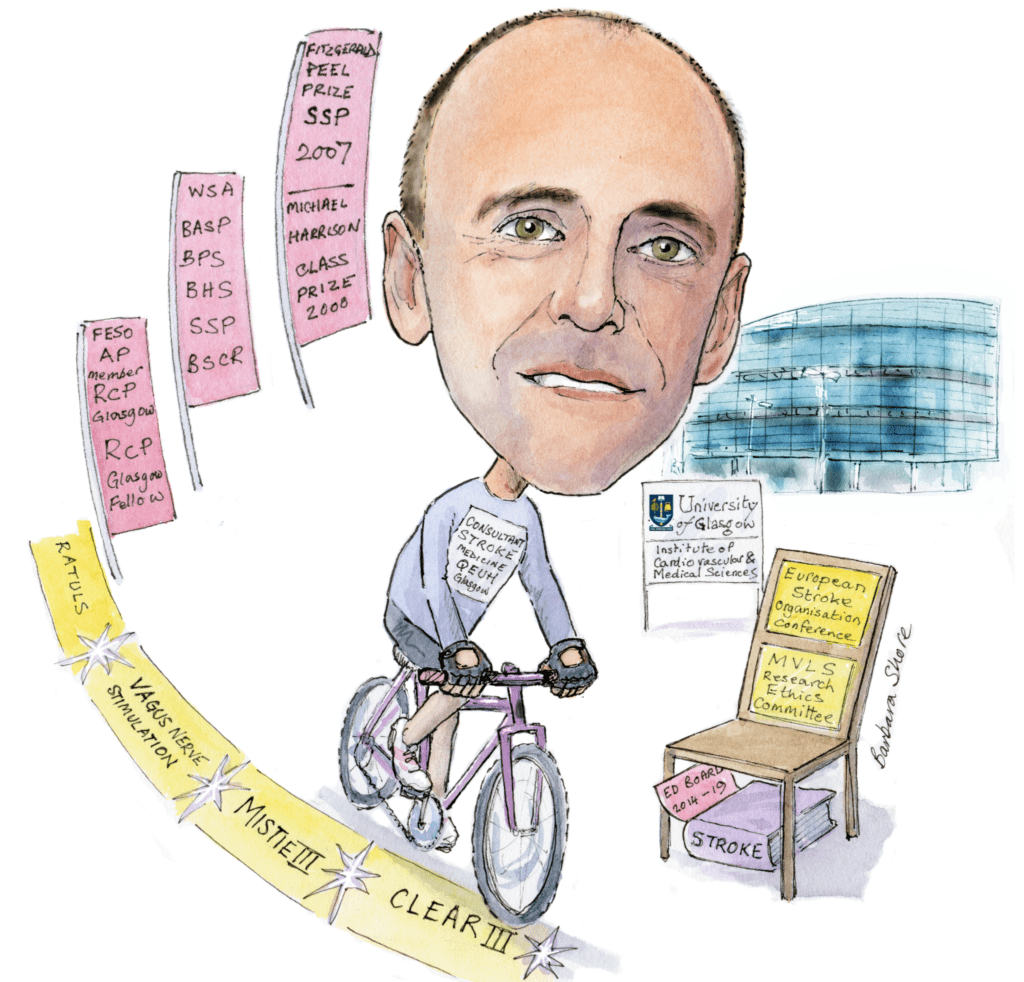
Fact File:
Clinical and academic appointments:
2017–Present: Professor of Stroke Medicine, Institute of Cardiovascular and Medical Sciences at the University of Glasgow, UK
2014–2017: Clinical Reader in Medicine, Institute of Cardiovascular and Medical Sciences at the University of Glasgow, UK
2011–2015: Consultant in Stroke Medicine and in Hypertension Clinic, Western Infirmary Hospital, Glasgow, UK
2011–2014: Clinical Senior Lecturer in Medicine, Institute of Cardiovascular and Medical Sciences at the University of Glasgow, UK
2007–2011: Clinical Lecturer in Medicine and Clinical Pharmacology in the Acute Stroke Unit/Institute of Cardiovascular and Medical Sciences at the University of Glasgow, UK. Specialist Registrar in Clinical Pharmacology and General Internal Medicine.
Society positions:
2018–Present: Chair, European Stroke Organisation Conference and co-chair joint ESO-WSO congress.
2018–Present: Treasurer, Scottish Society of Physicians
2017–Present: Executive committee, Association of Physicians
2015–Present: Chair, MVLS Research Ethics Committee
2014–2019: Editorial Board for Stroke
2014–2018: Committee member, British Association of Stroke Physicians
Current research:
- Altered extracellular vesicle microRNA expression in ischaemic stroke and small vessel disease
- Robotic therapy for upper limb recovery – RATULS
- Allopurinol for the prevention of stroke – XILO-FIST
- Vagus nerve stimulation paired with upper limb rehabilitation after chronic stroke: A blinded randomised pilot study









