The first European study to evaluate the economic impact of first-pass effect (FPE) found that FPE patients not only benefit clinically, they also endorse favourable economic outcomes. At the 15th Congress of the World Federation of Interventional and Therapeutic Neuroradiology (WFITN; 21–25 October, Naples, Italy), Tommy Andersson of Karolinska University Hospital, Stockholm, Sweden, and AZ Groeninge, Kortrijk, Belgium, concluded: “Based on these results, FPE may represent a new and valid goal for endovascular therapy in acute ischaemic stroke.”
The clinical and economic impact of first-pass success was assessed from a European cost perspective in conjunction with Cerenovus, using the results from the ARISE II (Analysis of revascularisation in ischaemic stroke with EmboTrap) study. Specifically, the investigators found that both hospitalisation-related and annual care costs were in favour of the FPE patients, a finding that persisted throughout the six countries they studied: France, Germany, Italy, Spain, Sweden and the UK.
In terms of the first-pass success rate in the target population, Andersson said that of the 227 patients included in ARISE II, 172 achieved a modified treatment in cerebral ischaemia (mTICI) score of 2c–3. Of these, 91 patients achieved first-pass success (FPE group), whereas for 81 patients multiple passes were needed (non-FPE group), giving rise to a 53% rate of FPE among patients in whom mTICI 2c–3 was achieved. He added that baseline characteristics were balanced across most variables between these two groups.
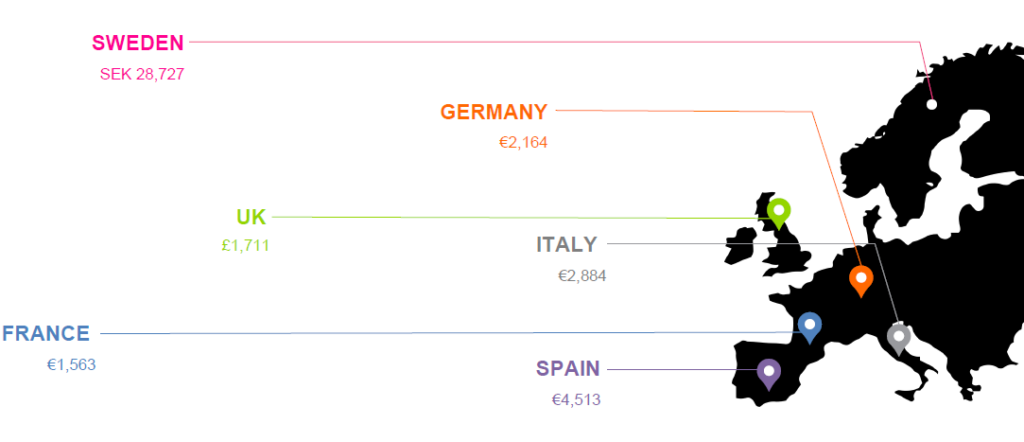
“Cost consequences were compared between the FPE group versus the non-FPE group, at two separate time-horizons,” Andersson said. Regarding hospitalisation-related economic impact, cost savings were derived from hospital length of stay and devices / methods used. The estimated cost savings for the FPE group were SEK28,727 (Kronor) in Sweden, €2,164 in Germany, £1,711 in the UK, €2,884 in Italy, €1,563 in France, and €4,513 in Spain.
Andersson also reported the annual care economic outcomes, which described the cost savings within the first year after stroke. Again, first-pass success led to further cost savings of SEK12,777 in Sweden, £2,041 in the UK, €694 in Italy and €2,140 in France.
Importantly, Andersson highlighted that the average cost for annual care in this first year following stroke incrementally increased as the modified Rankin Scale (mRS) score of the patient group increased. For example, costs for those achieving an mRS of 0 were €12,870 in France, and even though a significantly lower percentage incurred an mRS of 5, costs rose to €40,313 per patient for this cohort.
Speaking of the sensitivity analyses addressing the variability of different key parameters of the cost calculation, Andersson said: “The results were consistent with the main analyses regarding hospitalisation-related and annual care costs.” He added that variations in the total length of stay or increasing/decreasing the costs by 20% did not alter the direction of the results.
Andersson concluded, “Patients in the FPE group had improved functional outcomes, a trend towards lower mortality, and a faster and more complete recovery, which all led to reduced hospitalisation-related and annual care costs in every country that we studied.”
Now, speaking to NeuroNews, he outlines the importance of FPE: “It is clear that FPE leads to better clinical outcome which now has been shown to also save costs but we still do not fully understand exactly why it is so important.
“FPE mostly leads to a shorter procedure time, but that is probably not the complete truth. For instance, if it takes 45 minutes to achieve FPE, does it still have the same beneficiary effect? That may very well be the case and consequently we need to develop even better techniques and strategies to be able to remove also difficult clots, rich in dense fibrin and platelets, regularly with only one pass. We realise more and more that when performing a thrombectomy we have to immediately ‘throw in everything’ to achieve FPE. It is good for the patient and it probably also saves money.”









