By Kyriakos Lobotesis

To date, five randomised controlled trials have demonstrated the clinical benefit of endovascular therapy compared with intravenous (IV) tissue-type plasminogen activator (t-PA) in acute stroke. However, the economic evidence evaluating stent retrievers is limited. Kyriakos Lobotesis and others therefore set out to compare the cost-effectiveness of IV t-PA alone versus mechanical thrombectomy and IV t-PA in the context of the UK National Health Service.
The study, recently published in the journal Stroke, demonstrated that although the upfront costs for thrombectomy are high, the potential gains in quality-adjusted life years make the procedure cost-effective. This is a very central factor to consider when deciding whether to commission this clearly beneficial for acute stroke patients interventional service.
The decisions to implement new medical technologies and healthcare services are increasingly being made while taking into account economic considerations, such as cost, affordability and budget impact for which a health economic study is usually needed. Recently, five randomised controlled trials demonstrated the clinical superiority of adjunctive mechanical thrombectomy versus IV t-PA alone in acute ischaemic stroke. Previous economic evaluations of mechanical thrombectomy have been undertaken but have been based in the USA and on a range of outdated mechanical devices, all now superseded by stent retrievers. This new generation of thrombectomy devices has demonstrated a higher recanalisation rate and a better clinical outcome. More importantly, this is in patients with a stroke secondary to a large vessel occlusion who are known to have very poor outcomes.
Ischaemic stroke is the third highest cause of death and the leading cause of disability in the United Kingdom. Its overall incidence is postulated to increase and the economic burden of stroke is estimated to be £9 billion per year in the UK (it is US$38 billion in the USA). Stroke itself is an expensive disease in terms of its personal, healthcare and societal impact. The clinical value and effectiveness of thrombectomy is guided by the benefits, risks and costs associated. It has been suggested that although the upfront costs of thrombectomy are high, the potential reduction in morbidity can result in savings downstream, resulting in a significant reduction in the overall economic burden from stroke. The purpose of this study was to investigate the cost-effectiveness of mechanical thrombectomy in hyper acute stroke in the UK, based on a meta-analysis of the data recently published five randomised control trials.
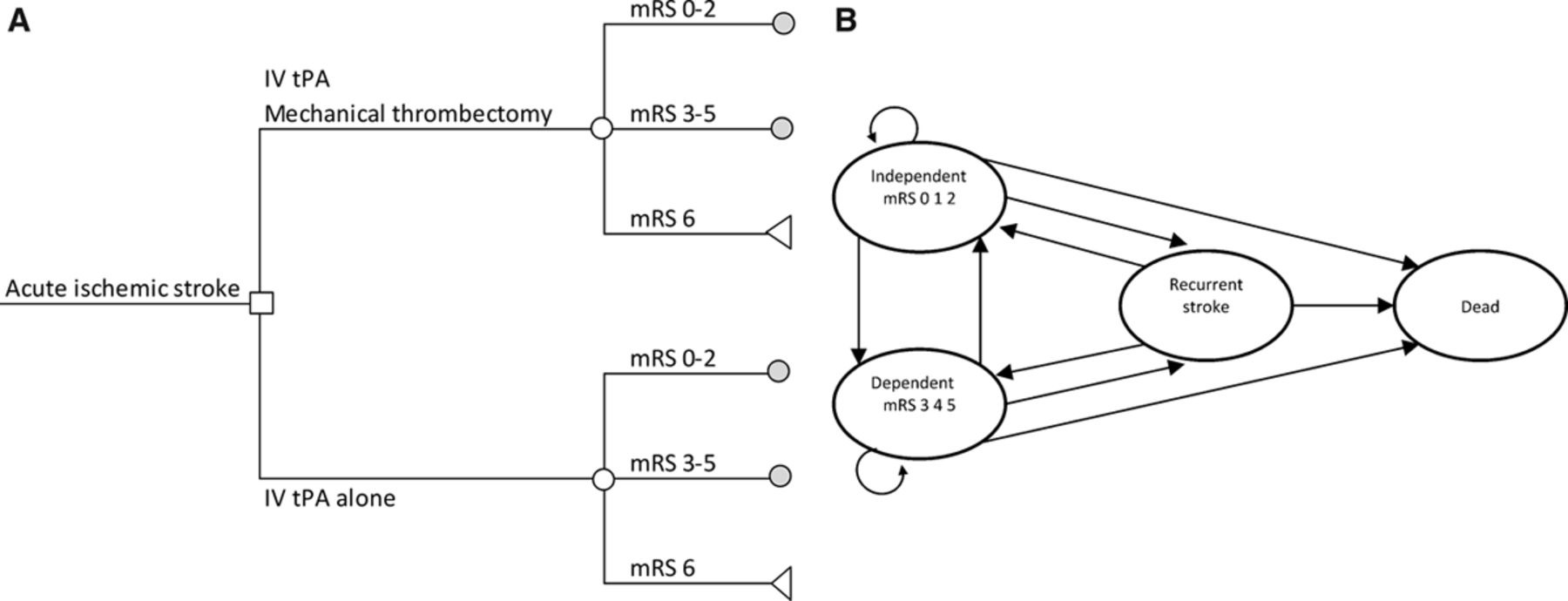
A cost-utility analysis was carried out with outcomes measured in terms of quality adjusted life years (QALYs). The number of deaths averted was also looked into as an additional outcome measure. A short term model was used to analyse the data on costs and clinical outcomes within three months with patients falling into one of three possible health states (see Figure A). A long-run Markov model was then used to estimate the expected costs and outcomes over a life-time horizon of 20 years (see Figure B). Two treatment options were considered, IV t-PA alone versus mechanical thrombectomy and IV t-PA. For both strategies, outcomes were based on modified Rankin Scale (mRS) scores measured at 90 days after stroke, which were assumed to be affected by recanalisation rates and symptomatic haemorrhage rates. The analysis was undertaken from the perspective of the UK National Health Service and Personal Social Services. Costs were calculated in 2013–2014 UK£ and are presented in US$.
The cost of the mechanical thrombectomy was estimated to be US$13,803 (£8,365), including the cost of the stent, the materials, and the procedure. The cost of IV t-PA was estimated to be US$2,953 (£1,214). The costs for the acute management of patients in the first three months after stroke and the following ongoing annual costs were taken from published reports. Acute and ongoing costs differed according to the level of disability, measured by mRS score. Acute costs include the length of stay in the Hyper Acute Stroke Unit, in the Acute High Dependence Unit, and in the rehabilitation ward, as well as the supported discharge cost and community care costs. The cost of a recurrent stroke was also assessed. Because it is not possible to predict the type and severity of a recurrent stroke, the cost to treat a recurrent stroke was calculated as the mean expected cost to treat an average stroke that may not need thrombolysis or thrombectomy.
The study demonstrated that mechanical thrombectomy following IV t-PA was associated with an incremental cost of US$12,262 (£7,431) and a gain of 1.05 QALYs per patient over 20 years. The additional costs were due to the cost of the procedure and device. QALYs were higher for mechanical thrombectomy because in the clinical trials used in the analysis, patients were more likely to have a better outcome and be independent (mRS 0,1,2). Assuming a cohort of 1,000 patients, the number of deaths over 20 years was 787 in patients treated with IV t-PA alone and 716 in patients treated with thrombectomy. Therefore, mechanical thrombectomy averted 71 deaths over 20 years. The incremental cost-effectiveness ratio of mechanical thrombectomy compared with IV t-PA was US$11,651(£7,061) per QALY gained. The results of a sensitivity analysis also showed that thrombectomy was cost-effective up to the cost to US$33,000 (£20,000).
Although the cost of thrombectomy is higher than that of IV t-PA initially, it leads to savings downstream in the stroke care pathway because of better outcomes. The difference between mRS scores can have a huge impact on the long-term healthcare costs, including societal costs. Obviously the cost effectiveness of thrombectomy is greatest in patients that improve clinically the most at three months. Between January and March 2014, 19,638 new cases of stroke were registered in the United Kingdom; 87.3% were ischaemic strokes and 11.5% had thrombolysis. Fifteen per cent of ischaemic strokes registered an acute large vessel stroke with an NIHSS score >16; therefore, thrombectomy could potentially be performed in 20% of patients who had thrombolysis. This means that in one year, around 1,800 patients could have had a thrombectomy, for an incremental cost (budgetary impact) of US$22 million (£13.4 million).
Summary
The principle finding of the study was that mechanical thrombectomy following IV t-PA, for acute large-vessel ischaemic stroke, saves one life for every 14 thrombectomies performed. It also significantly reduces disability and hence is cost-effective when compared with IV t-PA alone. We hope that this study will supplement the recently published randomised controlled trials but more importantly, will assist healthcare commissioners regarding purchasing and investing in this new but essential aspect of acute stroke services.
Kyriakos Lobotesis is at Imperial College London, UK













