A high sensitivity blood test might help doctors rule out traumatic intracranial injuries like brain haemorrhage and contusion before resorting to CT scanning, according to a large, multicentre observational trial published in The Lancet Neurology.
The novel blood test was administered within 12 hours of a suspected traumatic brain injury (TBI), and measured levels of two biomarker proteins which are released into the bloodstream following a brain injury. In the study, the test correctly identified 99.6% of patients who did not have a traumatic intracranial injury on head CT scans among over 1,900 adults (mostly with mild TBI) presenting to emergency departments in the USA and Europe.
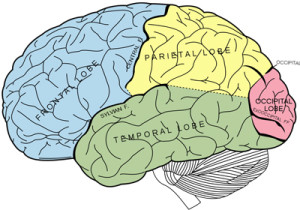
Current practice for mild TBI involves a series of checklists of symptoms and signs—known as clinical decision rules—that a treating physician will look for to decide whether a CT scan is necessary. One of the most important clinical guides for determining the need for a CT scan is the patient’s initial level of alertness—measured using the Glasgow Coma Scale score (GCS)—with some guidelines recommending a head CT for anyone with a less than perfect GCS score of 15.1
The blood test investigated in this study was able to predict which patients did not have a brain injury visible on CT scan with very high accuracy, even among those with a GCS less than 15. Further research to determine the extent to which the biomarker test complements decision rules, and as well as its impact on health care costs and patient throughput, will be key to understanding the test’s usefulness in clinical practice.
“Based on the results of this multicentre study, routine use of the new biomarker test in emergency departments could reduce head CT scans by a third in acutely head injured patients thought to be in need of CT scanning, avoiding unnecessary CT-associated costs and radiation exposure, with a very low false-negative rate”, says Dr Jeffrey Bazarian at the University of Rochester School of Medicine in Rochester, New York (USA) who co-led the research.2
Our results suggest that patients with mild TBI (initial GCS of 14 or 15) who have no other indication for a CT (such as a focal neurologic deficit), and who have a negative test can safely avoid a CT scan. Those patients with a positive test have a 10% chance of an intracranial lesion and most clinicians would get a CT scan of their head to determine if an intracranial injury exists, and define it further. The extent to which these biomarker results can be applied to patients presenting with more severe injury, that is in those with a GCS less than 14, requires further confirmation.” 2
Based on early, unpublished results of the study, the US Food and Drug Administration has approved the commercial use of this blood-based brain biomarker test, making it the first clinically approved test of its kind in North America.
TBI occurs when an external force such as a bump or blow to the head disrupts the normal function of the brain. Leading causes include falls, motor vehicle accidents, and assaults. An estimated 54–60 million people worldwide suffer a TBI every year. In the USA, TBI is responsible for more than 2.5 million visits to the emergency department every year, most of which involve milder TBIs like concussion.
Currently, doctors use CT scans to detect traumatic intracranial injuries, usually bleeding, which sometimes require immediate neurosurgery. Over 20 million head CT scans are performed each year in the US alone. However, CT scans reveal such injures in less than 10% of those with milder head injuries, which make up three-quarters of all TBIs, and there is concern about the high radiation dose associated with CT scans of the head which can increase the risk of cancer.
Previous research has highlighted the potential of blood-based brain injury biomarkers to predict patients at high risk of intracranial injuries and in need of CT scanning. S100B is a well-accepted biomarker for TBI and is already in clinical use in Europe. Two other proteins—ubiquitin C-terminal hydrolase-L1 (UCH-L1) and glial fibrillary acidic protein (GFAP)—have also emerged as promising predictors of head CT results in small studies.
To provide more evidence, the researchers conducted a prospective study of 1959 adults (aged 18 or over) attending emergency departments between December 2012 and March 2014 with suspected TBIs at 22 sites in the USA and Europe. The ALERT-TBI study directly compared the results of the new biomarker test combining UCH-L1 and GFAP with head CT scan results.
Participants had a Glasgow Coma Scale score ranging from 9-15, and the majority (98%) had a mild TBI, with a score of 14–15 (GCS scores range from 3 [deep coma] to 15 [full consciousness]). All participants received a head CT as part of standard emergency care and had blood samples taken within 12 hours of injury.
Results showed that 125 (6%) of participants had intracranial injuries detected on CT and eight (˂1%) had injuries that were neurosurgically manageable. 1288 (66%) of patients had a positive GFAP and UCH-L1 test result, and 671 (34%) had a negative result.
The new biomarker test was positive in 97.6% of patients with a traumatic injury on head CT scan (sensitivity), whilst the probability that a patient with a negative test result was truly injury free was 99.6% (negative predictive value).
Given that there were ten times as many positive GFAP and UCH-L1 tests as positive CT scans among patients with TBIs, the authors speculate that these two proteins may be detecting more subtle degrees of injury not visible on CT scans.
According to co-lead author Peter Biberthaler from the Technical University of Munich, Munich, Germany, “The majority of patients presenting with mild traumatic brain injuries like concussion do not have visible traumatic intracranial injuries on CT scans. Given the GFAP and UCH-L1 biomarker test’s inherent simplicity, requiring only a blood draw, and its reliability at predicting the absence of intracranial injuries, we are hopeful of its future role in ruling out the need for CT scans in these patients.”2
The authors note several limitations, including that the study did not evaluate the test’s predictive ability for clinical outcomes such as prolonged post-concussive symptoms, cognitive impairment, and decreased functional status. They also note that it did not attempt to assess the test’s diagnostic accuracy compared with currently used biomarkers (ie, S100B) and clinical decision rules for triaging CT scanning. Finally, the sensitivity analysis comparing the diagnostic performance of the biomarker test for each of the proteins separately suggested that GFAP alone might perform as well as the two proteins combined, and requires further validation.
Writing in a linked Comment, Andrew Maas from Antwerp University Hospital and University of Antwerp, Belgium and Hester Lingsma from Erasmus University Medical Centre in the Netherlands, note that “several scientific and clinically relevant questions remain unanswered, despite ALERT-TBI being a pivotal study in the quest for objective parameters to aid in the evaluation of TBI in emergency departments. They write, “the only clinically relevant question for any new diagnostic test in mild TBI is does the test add value (eg, better outcomes or reduced costs) to currently used biomarkers and decision rules?…Inexplicably, this evaluation was not done…Our interpretation is that the added value of the test in clinical practice might well be small or even absent, and we strongly encourage the authors to prove us wrong. That would constitute a true addition to science and clinical practice.”
Notes:
- Clinical decision rules were primarily designed to identify head injured patients with traumatic intracranial injuries requiring neurosurgery rather than identifying all intracranial injuries.
2. Quotes direct from authors and cannot be found in the text of the Article.