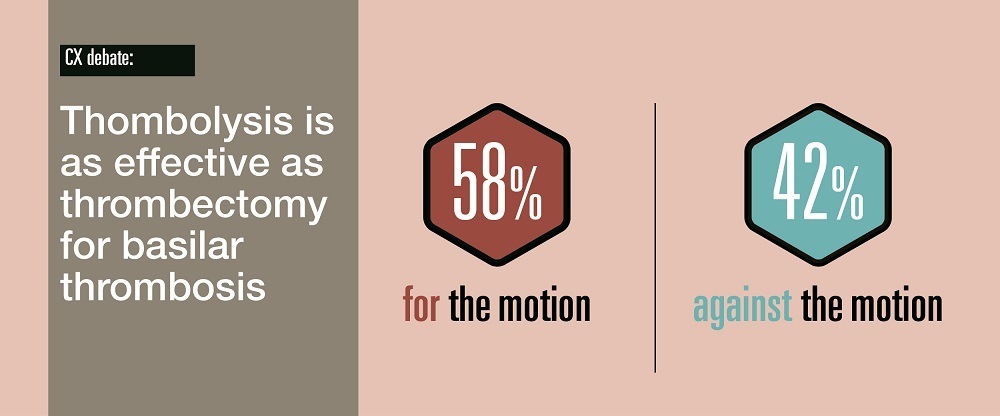
Thrombolysis is considered as effective as mechanical thrombectomy for the treatment of basilar artery occlusion (BAO)—despite existing evidence on both intervention options being limited. This is according to an audience poll conducted during the final day of the Charing Cross (CX) 2021 Digital Edition (19–22 April, online).
A debate entitled “Thrombolysis is as effective as thrombectomy for basilar thrombosis” was among the highlights from the online event’s Acute Stroke Controversies programme, and saw Wouter Schonewille, a neurologist at University Medical Center Utrecht (Utrecht, The Netherlands) argue in favour of the motion, while Shelley Renowden, a consultant neuroradiologist at the North Bristol NHS Trust (Bristol, UK) argued against.
Despite Renowden’s assertions that the degree and speed of recanalisation for BAO is “undoubtedly superior” with mechanical thrombectomy—particularly when using newer thrombectomy devices—the majority of the CX audience (58%) ultimately sided with Schonewille, following his suggestion that intravenous thrombolysis (IVT) is more appropriate in treating the majority of BAO patients, and thrombectomy should be reserved only for certain, more severe cases.
Schonewille kicked off the debate by claiming that, while numerous clinical trials have demonstrated the efficacy of endovascular thrombectomy (EVT) in treating acute ischaemic stroke patients with large vessel occlusion, most of these trials have excluded patients with BAO, meaning the results “cannot be extrapolated to these patients”. He also referenced the BASICS (Basilar artery international cooperation study) trial—of which the final findings were presented by Schonewille himself last year.
The trial found “no significant difference” in outcomes between the two treatment arms, which involved using EVT combined with best medical management (BMM), and BMM alone. Schonewille stated that IVT was found to be the best treatment option in patients with lower scores (<10) on the National Institutes of Health Stroke Scale (NIHSS), and concluded his presentation by adding that patients with BAO should be treated with IVT, while EVT should be limited to certain patients with a moderate or severe NIHSS score (≥10).
Renowden countered these points by arguing that, despite the problems some trials, including BASICS, have experienced with recruitment, “there is enough information to conclude that thrombectomy and the standard medical treatment is more effective than the standard medical treatment alone for BAO—for those with an NIHSS of 10 or higher within 6–8 hours of stroke onset”. In addition to the BASICS trial, Renowden also referenced the BEST (Acute basilar artery occlusion: endovascular interventions versus standard medical treatment) trial, and data from the Chinese BASILAR (Endovascular treatment for acute basilar artery occlusion) study, in which she claimed the outcomes for BAO patients who received EVT were “significantly better” than those seen in patients who did not receive EVT.
And, when questioned by Hugh Markus—one of the session’s moderators and a neurologist at the University of Cambridge (Cambridge, UK)—about which BAO patients she would deem suitable for thrombectomy, Renowden said it is important to consider various factors relating to the individual patient, including their age, NIHSS and Glasgow Coma Scale (GCS) scores, and ultimately what chance they have of achieving a “good, independent outcome”. However, despite her suggestions that EVT is safe and has demonstrated effectiveness in clinical trials, particularly among more severe stroke patients, Renowden’s argument only garnered 42% of the CX audience’s vote.
In the debate following their individual presentations for and against the motion, Schonewille and Renowden both alluded to the ongoing BOACHE (Basilar artery occlusion Chinese endovascular) trial, which differs slightly from previous studies assessing basilar artery occlusion in that it is concerned with interventions taking place at 6–24 hours after stroke onset, while other studies have primarily focused on delivering treatments within six hours.
The two speakers also agreed that, despite the limited evidence that is currently available, further randomised controlled trials comparing EVT to IVT are unlikely to be possible.
Both presentations, and the subsequent debate and audience poll, can be viewed online by CX registrants here.












