 William Mack is a professor of neurosurgery and vice-chair of academic affairs in the Department of Neurological Surgery at the University of Southern California (USC) Keck Medical Center, and the principal investigator and director of the Cerebrovascular Laboratory in the Keck School of Medicine’s Zilkha Neurogenetic Institute (Los Angeles, USA). He is also on the Board of Directors of the Society of NeuroInterventional Surgery (SNIS), where he served as president from 2020–2021. Mack discusses his career in neurointervention with NeuroNews.
William Mack is a professor of neurosurgery and vice-chair of academic affairs in the Department of Neurological Surgery at the University of Southern California (USC) Keck Medical Center, and the principal investigator and director of the Cerebrovascular Laboratory in the Keck School of Medicine’s Zilkha Neurogenetic Institute (Los Angeles, USA). He is also on the Board of Directors of the Society of NeuroInterventional Surgery (SNIS), where he served as president from 2020–2021. Mack discusses his career in neurointervention with NeuroNews.
What initially attracted you to medicine, and the field of neurointervention specifically?
I have always had an interest in science and medicine. My uncle is a paediatric cardiac surgeon and I have been fascinated by his work since I was a child. I became interested in neuroscience during college and medical school. I was very intrigued by how the brain works. Helping people during difficult times has always been appealing to me and I have a great sense of fulfilment knowing that the work I do has a profound impact on my patients’ lives. I was attracted to neurointerventional surgery because it gave me the opportunity to participate in a rapidly evolving, cutting-edge field of medicine that focuses on helping people during critical times. Being able to perform minimally invasive brain surgery is also something I find incredible.
Who have your mentors been and how have they impacted your career?
I have been fortunate to have a number of fantastic mentors that have helped shape my career, and there are several outstanding individuals that have been directly responsible for my training at various stages. My parents, Bill and Deena Mack, taught me the value of hard work, respect, and the importance of pursuing a job that I love. As a medical student and resident at Columbia University, I had the privilege of working in Sander Connolly’s laboratory. He is the epitome of a surgeon-scientist and a true inspiration. During residency, I had the opportunity to learn cerebrovascular and neuroendovascular surgery form Robert Solomon, Sander Connolly, Philip Meyers and Sean Lavine. They were each exceptional surgeons and caring doctors who taught me the importance of preparation, surgical discipline, and working in a collaborative team. During my fellowship, I learned from Fernando Vinuela, Gary Duckwiler and the University of California, Los Angeles (UCLA) team—true pioneers in the neurointerventional field who taught me the importance of innovation, biotechnology, and the need to constantly evaluate our treatments in a scientific manner. As a faculty member at USC, I have had the opportunity to learn every day from a master cerebrovascular surgeon, Steven Giannotta, and I have gained an appreciation for the amount of learning that can be done long after the formal training of residency and fellowship. I am also grateful to be able to learn each day from my partners Arun Amar, Jon Russin, Matt Tenser and Ashkan Mowla.
What has your experience been as the president of the Society of NeuroInterventional Surgery?
It has been a fantastic experience; both inspiring and humbling. I have had the chance to work with such an impressive group of people who are devoted to advancing the field of neurointerventional surgery. It is truly a great time to be involved with this specialty. The field is growing through multidisciplinary collaborations and innovation is occurring at a rapid pace. We have become large enough to have a voice that is heard across medical and leadership communities, and we have used this voice to advocate for our patients. Although we have accomplished so much as a group over the course of the year, it feels as if there is so much more that can be done—and the society must pick which important issues to focus its time and efforts on.
How has COVID-19 affected your work at SNIS over the past year?
COVID-19 has limited the ability of our teams to meet in person. We had to convert our annual conferences, board meetings and practical courses to virtual platforms. Our physicians were also unable to proctor new procedures in person for a period of time. Nonetheless, we carried out each of these events successfully in the “new normal”. This took a lot of planning from the organisers and administrative team, but it also showed us how adaptive we could be when we needed to. In some ways, we have become more connected with people who live greater distances away, and these advances will not go away after the pandemic. However, we have all missed the personal interactions and camaraderie of face-to-face meetings, and are very excited to congregate at the annual meeting in Colorado Springs this year.
What do you feel has been the most important development in the field of neurointervention during your career?
The success of the randomised controlled mechanical thrombectomy trials in 2015 and beyond was the most important development in the field of neurointervention during my career. I think that neurointerventional surgeons believed stroke to be a surgical disease early on. We had all seen up close the successes of the early mechanical thrombectomy procedures. It took some time to optimise device development and systems of care, but the resounding success of the 2015 trials convinced the rest of the medical profession. This is a procedure that has a “number needed to treat” that is far fewer than many of the most successfully treated diseases in all of medicine, and those trials demonstrated the power of collaboration and well-designed clinical trials around an innovative procedure with great benefit to our patients.
What is the most significant unsolved problem in the field right now?
Designing and implementing proper stroke systems of care is very important in our field right now. Getting our stroke patients to the right place the first time around is critical. We have the personnel, devices, and techniques, to effectively treat large-vessel ischaemic stroke and, while practitioners involved in acute stroke care have worked effectively in multidisciplinary teams, we now need to implement standardised transport and routing measures that ensure efficiency within the system. This is also the focus of the SNIS Get Ahead of Stroke effort.

What is your proudest achievement in the field of neurointervention?
Among my proudest achievements in neurointervention has been my participation in the collaborative and inclusive efforts that have been initiated and implemented by the SNIS board of directors over the past year. I take great pride in being a part of something that I feel will move our entire field forward on behalf of our membership and our patients. SNIS has worked with the Joint Cerebrovascular section of the American Association of Neurological Surgeons/Congress of Neurological Surgeons (AANS/CNS) and the Society of Vascular and Interventional Neurology (SVIN) to help establish objective and responsible fellowship guidelines, and is working towards implementing an organised fellowship match. In addition, the SNIS board of directors unanimously voted to create a new voting board position, the Diversity, Equity & Inclusion Chair, which will lead engagement with the SNIS membership in all aspects of diversity, and promote equity and inclusion within the society.
Besides your own work, what is the most interesting piece of neurointervention research you have seen in the past year?
The brain-computer interface work being done by Thomas Oxley and the team at Synchron is absolutely fascinating to me. The ability to help a person control motor function through their thoughts is incredible. Equally impressive is the ability to do so in a minimally invasive fashion via the blood vessels. The Stentrode device represents a move towards restorative neuroendovascular surgery as, rather than removing or treating existing pathologies, this technology will allow patients to recover function that was previously lost. This could be the beginning of a whole new field for neuroendovascular surgery and medicine.
What advice would you give to people embarking on a career in the field of neurointervention?
It is an unbelievable field. Progress is more rapid than in any other area of medicine. You can access the entire body, including the brain and spine, through the vascular tree, in a minimally invasive fashion—that is the basis of our specialty. The innovative tools that we use today will be replaced by newer, more effective devices that the members of our group help design and develop. We are treating diseases like subdural haematomas, and performing procedures like venous sinus stenting, that did not even exist several years ago. Neurointervention is an expanding field, our society membership is growing rapidly, and the impact factor of our Journal of NeuroInterventional Surgery is increasing substantially each year. If you want to work in an exciting and expanding field of medicine, neurointervention is the place to be.
What are your interests outside of the field of medicine?
I enjoy spending time with my wife, Courtney, and my five children—Jacob, 11; Daniella, 9; Charlie, 7; Lexi, 5; and Emma, 2. It is very busy in our household. We play sports, travel, and enjoy spending time with our extended family. Over the course of the past year, we have cooked themed dinners every Friday night that we eat together as a family. We have gotten creative in order to avoid any duplicates over the course of 50 weeks. We also have movie nights every Saturday and try to spend time outdoors together. In my free time, I like to ski, hike, swim and play golf too.
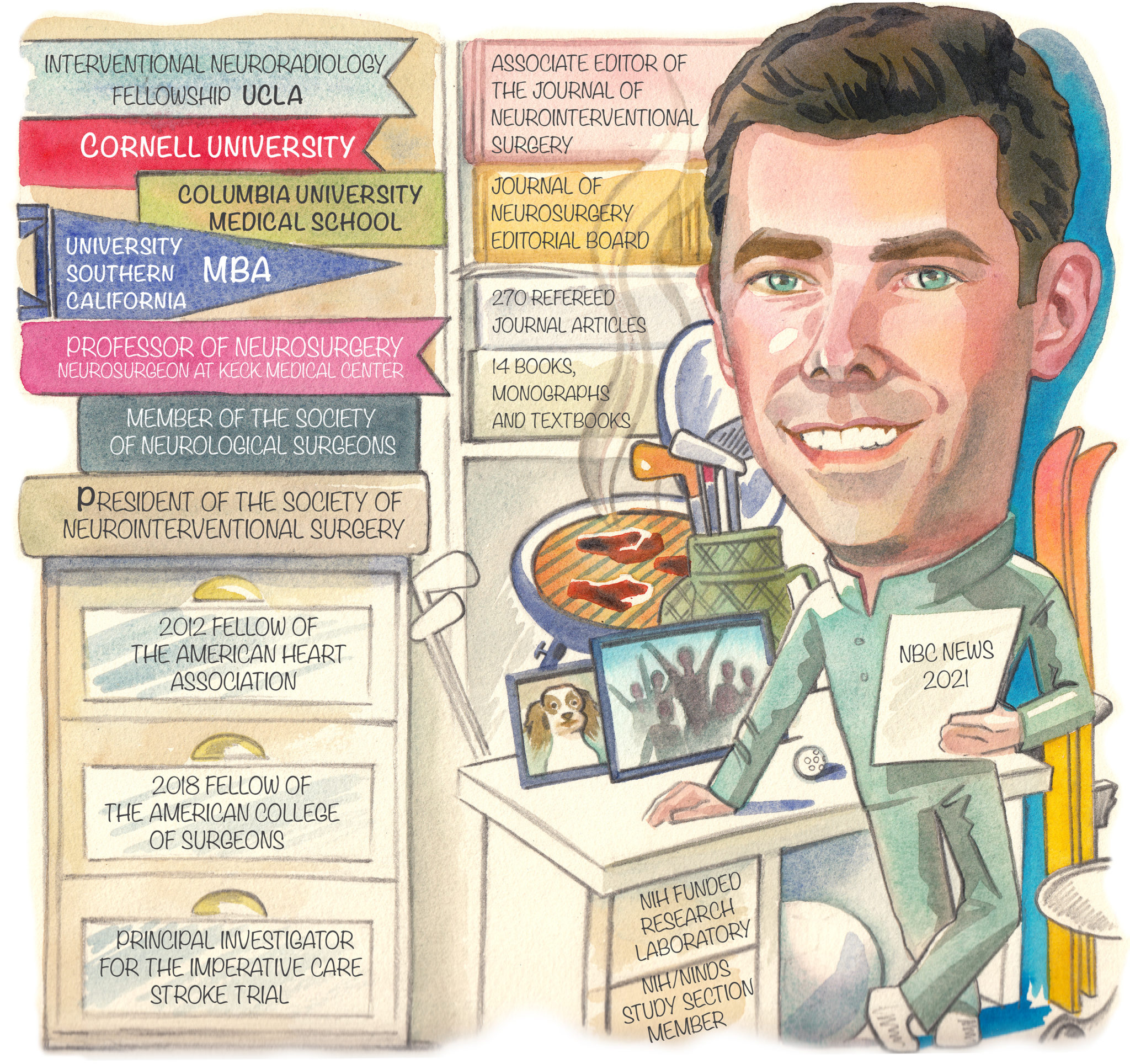
Fact file:
Current appointments:
- 2018–present: Professor of Neurosurgery and vice-chair of Academic Affairs, Department of Neurological Surgery, Keck Medical Center, University of Southern California (USC), Los Angeles, USA
- Principal investigator and director, Cerebrovascular Laboratory, Zilkha Neurogenetic Institute, Keck School of Medicine, University of Southern California (USC), Los Angeles, USA
Education:
- 1992–1996: BA, Neurobiology and Behaviour, Cornell University, Ithaca, USA
- 1996–2001: MD, Medicine, Columbia University College of Physicians and Surgeons, New York, USA
- 2011–2013: MS, Clinical and Biomedical Investigation, University of Southern California, Los Angeles, USA
- 2019–2022: MBA, Marshall School of Business, University of Southern California, Los Angeles, USA
Honours (selected):
- Fellow, American College of Surgeons (ACS), 2018
- USC Neurosurgery Teaching/ Mentorship Award, USC Department of Neurosurgery, 2019
- President, Society of NeuroInterventional Surgery (SNIS), 2020–2021
- Chair-elect, Cerebrovascular Section, American Association of Neurological Surgeons/ Congress of Neurological Surgeons (AANS/CNS), 2021–2022









