
Discussions at this year’s European Society of Minimally Invasive Neurological Therapy (ESMINT) congress (4–6 September, Marseille, France) revealed the extent of the disparities between the current regulatory systems in Europe and the USA, with experts and attendees outlining how “the tables have turned” over the past few years, potentially enticing more neurovascular device manufacturers to seek US Food and Drug Administration (FDA) clearance as their first port of call.
ESMINT past-president Christian Taschner (University of Freiburg, Freiburg, Germany) opened the session by disclosing the results from a survey of physicians working in the neurointerventional space. He noted that the “vast majority” of those who participated emphasised the significance of clinical evidence in their selection of new medical devices for endovascular procedures, and that—across three different scenarios presented to survey participants—prospective, multicentre registries and randomised controlled trials (RCTs) emerged as the preferred modalities for assessing new neurovascular devices.
Against this backdrop, two subsequent presentations examined certain components of the existing regulatory systems in the USA and Europe. Carlos Peña (The Jacobs Institute, Buffalo, USA) initially drew on his years of experience as former director for the Office of Neurological and Physical Medicine Devices in the FDA’s Center for Devices and Radiological Health (CDRH), advising ESMINT attendees to engage the FDA at an early stage, and attempt to utilise the regulator’s pre-submission process as a means for guiding product development and application preparation.
“If your strategy does not include a pre-submission step, it is probably not a very good strategy,” he stated, also highlighting the fact it does not cost anything for companies to engage in this voluntary process, and briefly extoling the benefits of the FDA’s Early Feasibility Studies (EFS) programme in discussion with session moderator Adnan Siddiqui (University of Buffalo/The Jacobs Institute, Buffalo, USA).
Following this, Miguel Antunes of the European Medicines Agency (EMA)’s Experts Panels and Groups Office outlined the main roles of the medical device expert panels set up under the recently introduced Medical Device Regulation (MDR). As part of the scrutiny mechanism for certain high-risk medical devices, he explained, the panels’ advisors issue an opinion on the assessment performed by notified bodies regarding clinical evaluation of a Class III implantable device, or a Class IIb active device for the delivery or withdrawal of a medicinal product.
The expert panels also serve advisory functions to several stakeholders—namely the European Commission, European Union (EU) member states, and manufacturers. Regarding the latter, the EMA reports having started a project piloting the provision of advice to Class III medical device developers on their clinical development strategy or clinical investigation proposals, as of February 2023. Antunes went on to draw attention to the fact that, during this pilot, no user fees are required to be paid and that it would be possible to submit a letter of interest for the second phase of the pilot until 15 September 2023.
European challenges
Despite this indication of a certain level of consistency between the two regulatory systems in the USA and Europe, discussions soon turned to the well-known setbacks observed following the introduction of the new MDR, and the challenges it has created for companies looking to gain clearance for their devices in the EU.
After acknowledging that it may be a somewhat “provocative” comment, Christophe Cognard (Toulouse University Hospital, Toulouse, France) noted that, currently, the process of gaining US FDA clearance appears to be less complex and generally easier than securing European approval for a neurovascular device. This prompted Hendrik Lambert, chief medical officer at Spanish medical technology firm Anaconda Biomed, to claim that “this is not just a provocative comment—it is true”.
Speaking to NeuroNews following this ESMINT session, Lambert elaborated that “the problems the MDR has created are multiple, and the combination of those problems has an exponential [negative] effect on the CE-mark certification of existing and new products”.

Chief among these problems, he continued, is the fact that all existing products—more than 500,000 devices and in-vitro diagnostics (IVDs)—that had been approved under the previous Medical Device Directive (MDD) are now losing their CE-mark and need to be re-approved under the MDR, requiring new clinical data.
“As there is no grandfathering option, even products that have been on the market for decades need to be recertified, although they are clearly safe and effective,” Lambert said. “It is very hard for those manufacturers to collect new data on long-lasting, existing products.”
Another ongoing challenges he highlighted is the fact that, under the MDR, all of the notified bodies in Europe have lost their licence and need to be recertified “after a very excessive auditing process lead by a combination of competent authorities”.
“As a consequence,” Lambert asserted, “the number of notified bodies that are currently approved is one third of the number it was before—from about 90 before MDR to slightly over 30 today. It is impossible to recertify such a high number of products with a strongly reduced number of notified bodies. The delays for certification are huge for both existing products and for new, unapproved products. For existing products, the original transition period was initially three years, but has now been extended several times to—currently—the end of 2027. For new products, a typical approval time is 1.5-to-two years. In the USA, for a 510(k) [clearance], it is three-to-six months or less.”
Explaining the root of this discrepancy, Lambert noted that the MDR considers any product used in the proximity of the heart or brain to be a Class III device. Thus, these products require high amounts of documentation—even if they are “simple and inherently safe” devices like catheters or guidewires. However, this is not the case in the USA, he added.
“Once the product is approved, there is an excess of documentation with clinical data required to be submitted periodically—mostly annually—for the full lifetime of the device,” he averred. “This is a very high burden for manufacturers, and a strong limitation on innovation. The MDR has created a lot of uncertainty around planning and the path to approval. Uncertainty is the biggest enemy to investors and, hence, innovation.”
“The tables have turned”
Further ratifying Cognard’s earlier point, Lambert also affirmed that many global companies—even those based in Europe—are currently more likely to favour seeking US FDA approval as a first port of call versus attempting to navigate the European MDR.
“The FDA has established powerful and transparent processes for EFS to stimulate innovation,” he stated. “Also, many products used in cardiology and neurointervention require a Class III certification process in Europe but can be cleared through a lighter 510(k) path in the USA. The road to approval in the USA is more predictable and, afterwards, it gives them access to a larger market compared to Europe.”
Weighing in on the discussion at ESMINT, session moderator Ajay Wakhloo, CEO and president of clinical-stage biotechnology firm Prometheus Therapeutics, offered yet another corroborating statement from a US perspective, noting that “we used to envy Europeans” when it came to medical device approvals. He also recalled having previously required compassionate use provisions—often referred to by the FDA as Expanded Access—in order to use CE-marked products to treat cancers, among other conditions.
“But, now, the tables have turned,” he continued. “The FDA in the USA has very clear guidelines and it is very easy to speak in advance about submissions.”
Wakhloo further asserted that, “in the modern era, we should be able to create a dictionary where both bodies speak the same language”, before adding that “there must be a way to simplify this”. Subsequently, Antunes clarified that the EMA plays a “very different” and “more limited” role in the regulation of medical devices compared to the US FDA. In terms of premarket assessment of medical devices, notified bodies “would probably be the rough counterpart of the FDA” in Europe, he added, also noting that—because it is anticipated that manufacturers may seek scientific advice in both the USA and the EU—ongoing discussions are taking place regarding possible future points for regulatory alignment.
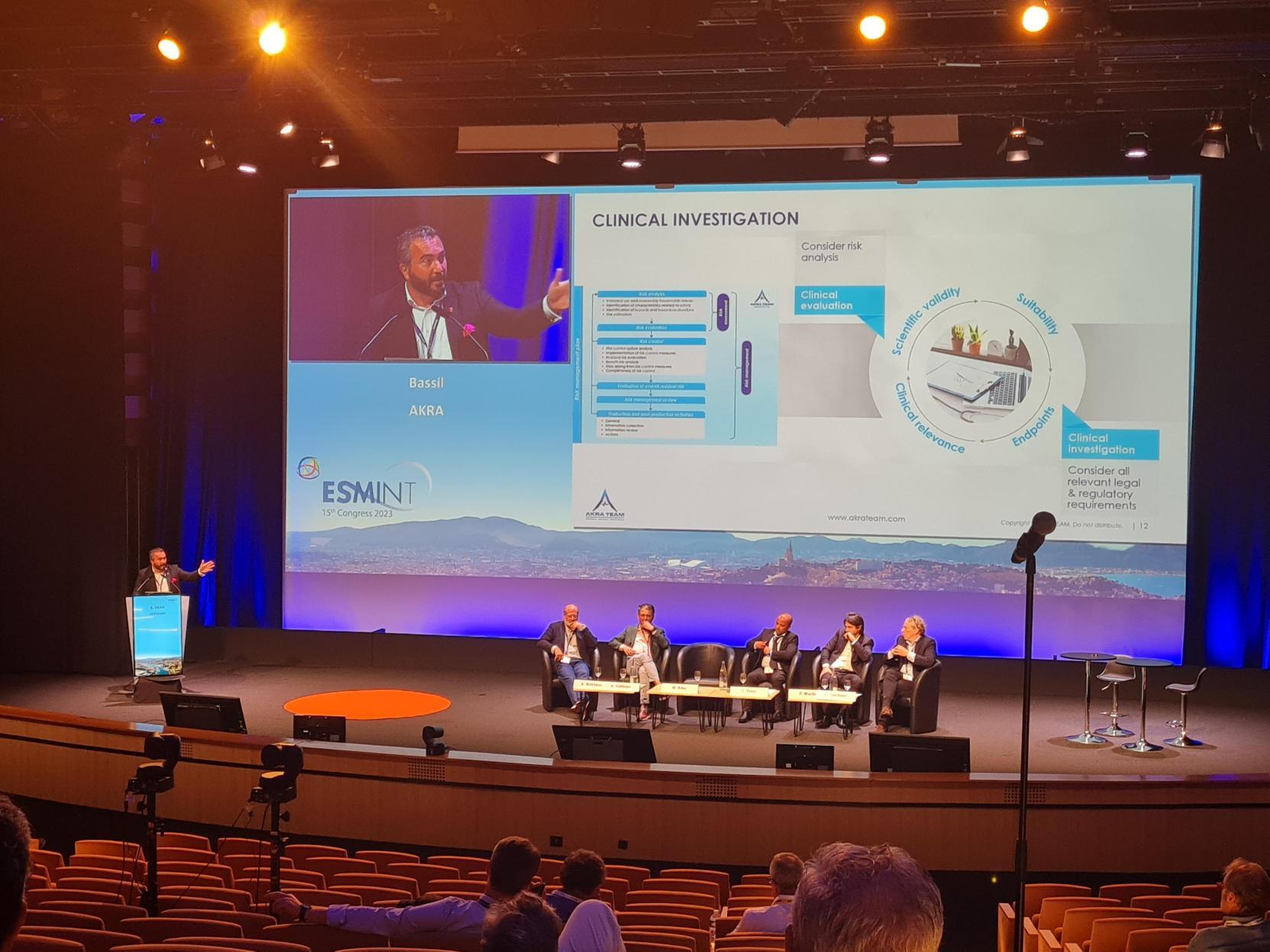
The session’s final presentation saw Bassil Akra, owner and CEO of global consultancy company AKRA TEAM, offer advice on how best to navigate a neurovascular device through the current European regulations. With the enduring challenges the EU MDR has raised in mind, he highlighted the benefits of ‘voluntary consultation’, whereby manufacturers can seek scientific insight from an expert panel for certain high-risk devices before undertaking performance evaluations and clinical studies.
A discussion following this presentation saw Akra agree with Antunes’ earlier point that notified bodies, rather than the EMA, are more comparable to the US FDA in Europe. Akra then built on this statement, encouraging the European Commission to empower notified bodies and make them even more like the FDA by ensuring they are involved in the early stages of regulatory pathways in order to make matters “clearer” for companies.
“It does not make sense,” he noted, “to have the EMA overseeing the final work of the clinicians at the notified body, but to have a single competent organisation or authority doing the assessment of the clinical and performance evaluations of devices—someone needs to be responsible!” And, commenting on the difficulties many manufacturers are currently encountering in Europe, he added: “I do not blame notified bodies—I blame the new system [MDR] and the expectations it brings.”
Akra also shone a spotlight on problems relating to the involvement of the designated authorities in member states who “bring a lot of inconsistency” to the implementation of EU requirements. “They create inconsistency on the EU level but also in their own member state by setting different expectations for the notified bodies depending on their size and establishment level,” he stated. “Too many cooks spoil the broth.”
A path forward?
Akra went on to posit that large-scale registries are likely to be of critical importance under the EU MDR moving forward—ideally, ones predicated on the same safety and performance criteria, in a standardised way, so as to establish a strong evidence base on the device in question. He pointed out that this would help in establishing a platform to support approvals and post-market surveillance of devices intended for vulnerable and/or limited patient populations.
Wrapping up the session, Siddiqui noted that “there is a lot of weight placed on precedence” under US FDA regulation, whereby manufacturers can cite previous examples of similar device approvals to support their case as well as interact with the agency on differences of opinion around the data.
This led Akra to highlight another discrepancy between systems in Europe and the USA right now: the fact there is no such process under the MDR. According to Akra, manufacturers can appeal to the European regulator as part of device classification disputes, but not when it comes to the actual regulatory, quality or clinical certification decisions on their product.
“You can appeal a decision made by a notified body,” he concluded, “but only to the same notified body—and they will already have formed their view. This is the problem created by a system having many contributors, including the EU Commission, designating authorities, [competent] authorities, notified bodies, and the EMA, but no full empowerment or responsibility for timely device availability on the EU market.”
Following ESMINT, Akra spoke to NeuroNews to offer the following advice to European device manufacturers: “They should read the MDR, request a pre-submission meeting with the notified body during which they inform them about their strategy, and get details regarding any administrative expectations that must be considered. Such a meeting is helpful to build relationships and understand expectations. They should not expect a pre-submission meeting like [those offered by] the US FDA, since notified bodies are not allowed to consult, but it is still important for building a relationship.”
And, when asked by NeuroNews to speculate on the short-term future of device regulation under the MDR, Lambert and Akra put forward somewhat differing perspectives.
“Unfortunately, no positive signs have been observed yet,” Lambert said. “I hope the European authorities will understand soon that a recertification of all existing products with a limited number of notified bodies cannot be sustained, and that certification of new products is a priority to ensure innovation in Europe. So far, we have not seen any sign from the authorities to put the MDR in question, or initiate a discussion with the related parties for modification or improvement.”
“The European system is currently undergoing a big shift, which needs to be assessed with a focus on the implications for the EU healthcare system, and availability of medical devices and IVDs to healthcare professionals and patients,” Akra added. “I personally believe that the system will balance again soon, since everyone knows that the intention of legislation is to ensure higher levels of safety and protection to the patient, by delivering effective devices. And overregulating might harm the patient and therefore [should] be avoided in the interest of a good, functioning healthcare system.”









