We have all heard the story. It goes like this…
“Once upon a time there were five brave randomised trials that went out into the big, wide world to fight IV-lysis and conquer the kingdom of stroke treatment.1-5 These trials demonstrated indisputable evidence that mechanical thrombectomy improves the outcome of patients suffering from a large vessel occlusion stroke. Since then, techniques for mechanical thrombectomy have evolved further, many other studies have confirmed the superiority of endovascular stroke treatment,6-16 and interventionalists around the world can now choose between a variety of methods which are both safe and effective. And from there on, all neurointerventionalists lived peacefully and happily ever after.
An idyllic story… But it may be time to look at the facts, writes Martin Wiesmann.
All the evidence from randomised trials in favour of mechanical thrombectomy comes from studies in which either all, or the vast majority of patients in the endovascular groups were treated using stent retrievers.
In these studies, endovascular treatment improved the outcome of stroke patients significantly. It is therefore safe to conclude that stent retrievers should be used as first-line treatment (Level 1A evidence).
There is considerable evidence that advanced techniques can further improve results of stent retriever thrombectomy.
To name just a few: Additional use of balloon-guide catheters,7,16 active push deployment technique,17 bare-wire thrombectomy technique,18 and SAVE technique.13 We have good reason to believe that these techniques will improve the outcome of our patients, and we should use them every time.
It is not true that mechanical thrombectomy per se improves the outcome of stroke patients.
There are numerous endovascular approaches including a variety of mechanical thrombectomy procedures and devices. All these techniques differ in their reperfusion rates, safety profiles, and clinical outcome results. The “unhappy triad” of the three negative endovascular stroke studies published in 201319-21 is a prime example of this fact. It is important to remember that these studies nearly killed the practice of endovascular stroke treatment. It is not enough to perform mechanical thrombectomy. We need to use a technique with proven benefit for patient outcome. More precisely, we are bound to use the technique which delivers best results in terms of patient outcome. Of all the “new” techniques, the most popular is direct thrombus aspiration (ADAPT) using large-bore distal aspiration catheters. However, the question remains, is ADAPT comparable to stent retriever thrombectomy?
It is not true that recent studies have shown that ADAPT is comparable to stent retriever thrombectomy.
The only randomised study comparing ADAPT plus IV-lysis with IV-lysis only (THERAPY) was negative.11 It did not show a significant difference in patient outcomes. The only randomised study comparing ADAPT to stent retriever thrombectomy was the recently published ASTER trial.9 This trial was negative, because it was designed to prove superiority of ADAPT (which was not observed), and because it was statistically underpowered to prove equality of methods.
But maybe we do not have to be so strict? Perhaps we can use reperfusion rates instead?
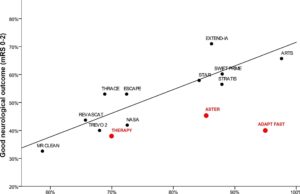
Vessel recanalisation has been shown to be one of the best predictors for good patient outcome. Indeed, if we look at the large trials using stent retriever thrombectomy [Figure 1; stent retriever studies shown in black] we find an almost perfect correlation between reperfusion rates and percentage of good patient outcomes (linear regression of stent retriever studies shown as black line; R2=0.873, p<0.001). Therefore, it could indeed make sense to use reperfusion rates as a proxy.
At this point we have to ask ourselves two important questions: Are reperfusion rates between ADAPT and stent retriever thrombectomy comparable? Is there any evidence that other factors except reperfusion rates play a role?
Although others may have a different opinion: I do not feel ADAPT has comparable success rates of vessel recanalisation to stent retriever thrombectomy.
The majority of stent retriever studies published in the last few years have reported reperfusion rates (TICI 2b-3) in a range from 65 to 100%.2-8,12-13 There are only three larger trials with comparably high quality in study-design using ADAPT as first-line technique.9-11 In these, reperfusion rates range between 70 and 95%. The ASTER trial, which is the largest and most recent ADAPT study, reported a reperfusion rate of 85%.9 This sounds pretty good, doesn’t it?
However, let’s look at the facts. The reperfusion rates in the ADAPT studies were achieved only because interventionalists were allowed to switch to stent retriever thrombectomy if direct aspiration failed. In the ASTER trial this was necessary in every third case in which thrombus aspiration was initially attempted (33%). Per study protocol, this means that in each of these patients three attempts at direct aspiration were performed without success. Subtracting those stent retriever cases reduces the true reperfusion rates of direct aspiration. In addition, I am convinced that every unsuccessful attempt produces downstream emboli, which may be too small to be visible, but certainly can impair patient outcome.22
But is this important? Maybe it does not hurt if we start with ADAPT, and later switch to stent retriever thrombectomy if required?
As long as vessels are recanalised at the end of the intervention, does it matter which technique was used? I believe this is absolutely of importance for our patients.
If we add the results of the ADAPT studies to Figure 1 (ADAPT studies shown in red), we observe two painful findings: 1.) At comparable rates of reperfusion, patients treated first by ADAPT had a lower chance for a good outcome. This means it definitely seems to make a difference which method is used first. 2.) There is no statistically significant correlation between reperfusion and patient outcome in the ADAPT studies (R2=0.391, p=0.744). This means that although the reported reperfusion rates in the latest ADAPT studies have improved, it has not improved patient outcome accordingly.
Conclusions:
Up to now, there is no statistical evidence that direct thrombus aspiration (ADAPT) improves patient outcomes, or is comparable to stent retriever thrombectomy.
The available studies suggest that ADAPT as first-line treatment may lead to worse patient outcomes as compared to stent retriever thrombectomy.
Perhaps the situation will be different in a few years. But until then, ADAPT should be performed in randomised studies only. We should not let ourselves be misled by angiographic images alone. It is patient outcome that matters.
There is level 1A evidence that stent retriever thrombectomy is effective in ischaemic stroke with large vessel occlusion. Thus far, stent retriever thrombectomy has demonstrated better patient outcomes. Therefore, stent retrievers should be used as first-line treatment.
References
- Berkhemer OA, Fransen PSS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015;372:11-20
- Jovin TG, Chamorro A, Cobo E, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 2015;372:2296-2306
- Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapidendovascular treatment of ischemic stroke. N Engl J Med 2015;372:1019-1030
- Campbell BCV, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015;372:1009-1018
- Saver JL, Goyal M, Bonafe A, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 2015;372:2285-2295
- Bracard S, Ducrocq X, Mas JL, et al. Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol 2016;15:1138-1147
- Zaidat OO, Castonguay AC,1 Gupta R, et al. North American Solitaire stent retriever acute stroke registry: post-marketing revascularization and clinical outcome results. J NeuroIntervent Surg 2014;6:584-588
- Pereira VM, Gralla J, Davalos A, et al. Prospective, multicenter, single-arm study of mechanical thrombectomy using Solitaire flow restoration in acute ischemic stroke. Stroke 2013;44:2802-2807
- Lapergue B, Blanc R, Gory B, et al. Effect of endovascular contact aspiration vs stent retriever on revascularization in patients with acute ischemic stroke and large vessel occlusion. The ASTER randomized clinical trial. JAMA 2017;318:443-452
- Turk AS, Frei D, Fiorella D, et al. ADAPT FAST study: a direct aspiration first pass technique for acute stroke thrombectomy. J NeuroIntervent Surg 2014;6:260-264
- Mocco J, Zaidat OO, von Kummer R, et al. Aspiration thrombectomy after intravenous alteplase versus intravenous alteplase alone. Stroke 2016;47:2331-2338
- Massari F, Henninger N, Lozano JD, et al. ARTS (aspiration–retriever technique for stroke): initial clinical experience. Interv Neuroradiol 2016;22:325-332
- Maus V, Behme D, Kabbasch C, et al. Maximizing first-pass complete reperfusion with SAVE. Clin Neuroradiol 2017; Feb 13. doi: 10.1007/s00062-017-0566-z
- Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016;387:1723–31
- Campbell BC, Hill MD, Rubiera M, et al. Safety and efficacy of Solitaire stent thrombectomy: individual patient data meta-analysis of randomized trials. Stroke 2016;47:798-806
- Mueller-Kronast NH, Zaidat OO, Froehler MT, et al. Systematic Evaluation of Patients Treated With Neurothrombectomy Devices for Acute Ischemic Stroke: Primary Results of the STRATIS Registry. Stroke 2017;48:2760-2768
- Wiesmann M, Brockmann MA, Heringer S, et al. Active push deployment technique improves stent/vessel-wall interaction in endovascular treatment of acute stroke with stent retrievers. J Neurointervent Surg 2017;9:253-256
- Nikoubashman O, Alt P, Nikoubashman A, et al. Optimizing endovascular stroke treatment: Removing the microcatheter before clot retrieval with stent-retrievers increases aspiration flow. J Neurointerv Surg 2017;9:459-462
- Broderick JP, Palesch YY, Demchuk AM, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med 2013;368:893-903
- Ciccone A, Valvassori L, Nichelatti M, et al. Endovascular treatment for acute ischemic stroke. N Engl J Med 2013;368:904-913
- Kidwell CS, Jahan R, Gornbein J, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med 2013;368:914-923
- Chueh JY, Puri AS, Wakhloo AK, Gounis MJ. Risk of distal embolization with stent retriever thrombectomy and ADAPT. J NeuroIntervent Surg 2016;8:197–202
Martin Wiesmann is professor of Neuroradiology and chair of the Department of Diagnostic and Interventional Neuroradiology at University Hospital RWTH Aachen, Aachen, Germany
Disclosure:Wiesmann is a consultant for: Stryker Neurovascular, SilkRoad Medical, Route 92 and has received reimbursement for lectures or travel support from Medtronic, Bracco Imaging, Siemens Healthcare and Stryker Neurovascular.
Acknowledgments:The author wants to express his sincere thanks to Drs Omid Nikoubashman and Anastasios Mpotsaris as well as to Ms Alena Gottmann, Ms Signe Haughton, Mr Toby Kent, Ms Ulrike Schlüter, and Ms Anne Lashinsky, for their assistance in the preparation of this manuscript.









