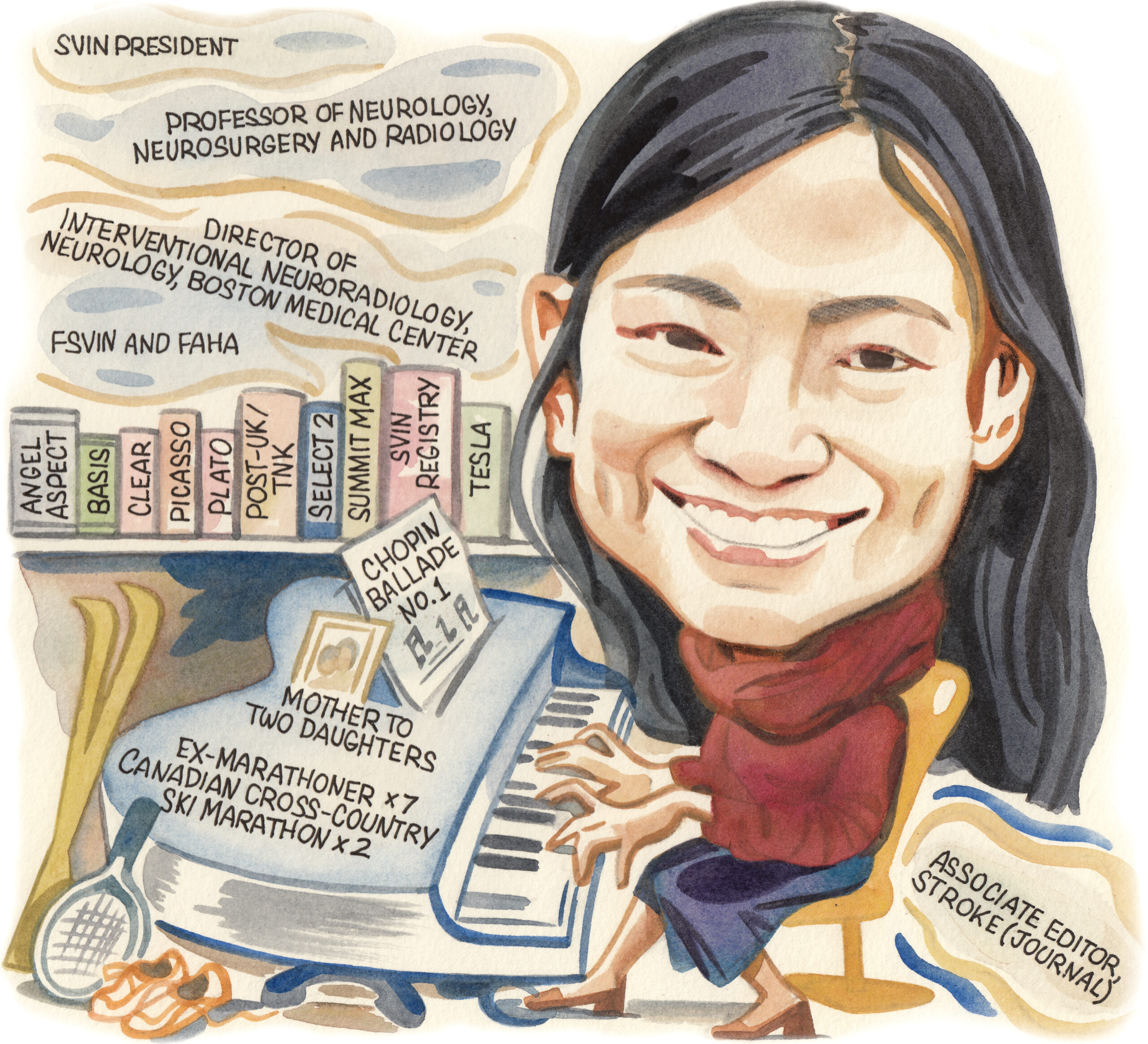
As one of six women currently leading major neurointerventional societies across the globe, Thanh N Nguyen (Boston, USA) is proudly playing a key role in challenging the medical field’s history of underrepresentation. In addition to her present tenure as president of the Society of Vascular and Interventional Neurology (SVIN), Nguyen is also professor of neurology, neurosurgery and radiology at Boston University Chobanian and Avedisian School of Medicine, as well as director of Interventional Neuroradiology and Interventional Neurology, and attending physician in the Vascular Neurology Service, at Boston Medical Center. Here, Nguyen speaks to NeuroNews about her neurointerventional mentors, ongoing efforts to boost gender equity in the field, and the most impactful clinical studies she has contributed to, among other topics.
What initially attracted you to medicine, and the field of neurology specifically?
I was drawn to medicine by my father, who was a primary care physician. The interest was to help people, understanding it would be a great privilege to learn and think about patient symptoms and physical signs. I became interested in neurology during medical school when I had the chance to learn, from my neurologist teacher Colin Chalk at McGill University (Montreal, Canada), how to perform a history and physical exam. Fascinated with the nervous system, it was then that I knew this is what I wanted to study.
Who have your most valued mentors been and how have they impacted your career?
I have been fortunate to have many mentors, foremost of whom are my piano teacher Luba Zuk, as well as neurointerventional mentors Jean Raymond, Alexander Norbash, Osama Zaidat and Raul Nogueira. Luba taught me the importance of a work ethic with daily piano practice and how to communicate music with an audience. Jean Raymond, Daniel Roy, Alain Weill and Francois Guilbert—my fellowship teachers—were instrumental in teaching me the simplicity, rigour and art of the neurointerventional field. I also learned about scientific writing and the importance of pragmatic trials from Jean. He believed that randomisation should be part of our clinical practice and that, with or without funding, it was our imperative to find the answers of how best to treat our patients through randomisation. My first papers with Jean were a sea of red lines. Jean was my harshest and toughest critic, which has helped me build to how I write today. Osama Zaidat gave me my first multicentre research project from the NASA registry, from which my confidence in research sprouted. Raul Nogueira was my senior resident, from whom I drew inspiration and guidance in neurointerventional research.
You are currently midway through your tenure as SVIN president—could you outline your experiences to date and your future aspirations in this role?
It has been a terrific journey and learning experience to serve as SVIN president. I have been fortunate to have a great team with our SVIN officers, board of directors, and committee chairs and vice-chairs. During my time as president, we have learned the importance of governance to empower our colleagues and our youth to succeed, lead and grow in synergy. I have had the pleasure to meet and work with a broad array of volunteers from our society, committee leaders, and the community at large. Our SVIN volunteers and our committee leaders are our bedrock. They drive the many missions of our society forward. Some of these experiences to date including the development of the SVIN-Stroke Interventional Lab Certification (SILC) initiative, in conjunction with Mission Thrombectomy. We acknowledge the importance of recognising and advocating for SILC labs globally. Fawaz Al-Mufti, our SVIN Mission Thrombectomy chair, has done a terrific job representing SVIN at the United Nations. We have had a terrific streak of educational platforms via the ‘WebNIRs’ and Virtual Stroke Academy, led by Krishna Amuluru and Amanda Jagolino-Cole. Over the next few months, we are rolling out brief practice updates and SVIN guidelines—you can be on the lookout for these in Stroke: Vascular and Interventional Neurology, our SVIN journal! And, the best is yet to come, as our annual meeting (20–22 November 2024, San Diego, USA) is around the corner, led by Alexandra Czap with a stellar lineup of speakers and innovation.
You are the first woman president of SVIN in its 18-year history. What impact do you think this will have?
Our field has an underrepresentation of women. We are now at an inflection point, with six neurointerventional societies being led by women—SVIN, the Society of NeuroInterventional Surgery (SNIS), the European Society of Minimally Invasive Neurological Therapy (ESMINT), the Asian-Australasian Federation of Interventional Therapeutic Neuroradiology (AAFITN), the American Association of Neurological Surgeons (AANS)/Congress of Neurological Surgeons (CNS) Cerebrovascular Section, and the Argentine College of Neurointerventionists (CANI). It is our collective hope that this will draw more women to our field. In addition, under the leadership of Robin Novakovic-White, the multisociety women’s group—where we forge common areas of discussion, collaboration and communication between women leaders across multiple societies—was initiated this past year. Dr Novakovic-White has also developed a women’s speaker registry so that conference organisers can refer to a list of women speakers, along with their area of expertise, as they plan their meetings.

Why is it necessary for neurologists, neurosurgeons, radiologists and other relevant specialties to cooperate and work together effectively, and how can this be achieved?
The advancement of our field draws from the collective strengths of the expertise and knowledge that each of our colleagues bring across multiple disciplines. This can be achieved by encouraging a collaborative environment of equity and sharing, whether it be from our shared advocacy efforts, educational outreach, or research collaborations.
What do you feel has been the most important development in the field of neurology during your career?
As many would agree, the most important advancement in the field of neurology has been the development and implementation of mechanical thrombectomy to decrease disability in patients with acute stroke secondary to large vessel occlusion. The abilities to embolise an aneurysm or pseudoaneurysm with coils, or embolise a dural fistula or chronic subdural haematoma without having to do open surgery, have also been remarkable innovations for our field.
Which of the studies you have been involved with do you believe has had the greatest impact on neurointerventional care?
I have been fortunate to be involved in many innovative and high-impact trials and projects, including ABBA, ACTION-CVT, ADJUVANT, ANGEL-ASPECT, ANGEL-REBOOT, ANGEL-TNK, ARAMIS, ASSET-IT, ATTENTION, ATTENTION-IA, BASIS, BRIDGE-TNK, CLASS, CLEAR, ESCAPE-MeVO, Global COVID SVIN Registry, MARVEL, PICASSO, PLATO, POST-TNK, POST-UK, REACT, RESCUE-BT, RESCUE-ICAS, SELECT2, SUMMIT MAX, SVIN Registry, TATUM, TEAM, TESLA, TOBAS, and TRIMIS. I believe that the CLEAR (Computed tomography [CT] for late endovascular reperfusion) study has had an impact on neurointerventional care, based on anecdotal feedback I’ve received, as it has enabled sites—particularly those with no access to perfusion imaging—to have data to show that treatment of patients with thrombectomy in the late window, as selected by non-contrast CT and CT angiography (CTA), conferred equally good outcomes compared to patients selected with advanced CT perfusion or magnetic resonance imaging (MRI). And, we recently showed, with data published in the journal Neurology, that treating these patients with non-contrast CT and CTA selection had twice the odds of good outcomes compared to the medical management of these patients.
Besides your own work, what is the most interesting piece of stroke research you have seen in the past year?
I was intrigued by the TRACE III trial, wherein patients with an arterial occlusion presenting in the 4.5-to-24-hour window who had no access to thrombectomy but had salvageable tissue were shown to have better outcomes when treated with intravenous tenecteplase compared to those who were medically managed. This offers a ray of hope for treating patients where systems of care or their economic circumstances do not permit thrombectomy access.
Looking ahead, which technologies or studies do you feel are likely to have the most significant impact on the treatment of neurovascular diseases?
There are many exciting innovations that are under development or in clinical trials. The Cerevasc endovascular shunt developed by Carl Heilman and Adel Malek is a novel way to divert cerebrospinal fluid into the venous system for patients with communicating hydrocephalus, without having to place a ventriculoperitoneal shunt. Brain-computer interfaces have the potential to restore function to patients affected by amyotrophic lateral sclerosis, stroke or spinal cord injury. Nanoparticles developed by Euphrates are a novel way to break up distal clots that may not be amenable to treatment with current endovascular techniques.
What advice would you give to people embarking on a career in the field of neurology?
It is important to keep an open mind and continue to learn the broad specialties of medicine—even if you know that you want to go into neurology. There are many intersections between medicine and neurology, so learning broadly will serve as a strong foundation base upon which you build your clinical skills.
What are your interests outside of the field of medicine?
Playing piano, playing tennis, and spending time with my daughters. Also, in my earlier years, marathon running—but my knees gave out after the seventh marathon—and cross-country skiing.
What is your favourite song to play on the piano?
Ballade No. 1, Opus 23, by Frédéric Chopin.
FACT FILE
Current appointments:
- 2023–present: President, SVIN
- 2019–present: Professor, Neurology, Neurosurgery and Radiology, Boston University Chobanian and Avedisian School of Medicine
- 2007–present: Director, Interventional Neuroradiology and Interventional Neurology, Boston Medical Center
Education:
- 2005–2007: Fellow, Interventional Neuroradiology, University of Montreal Hospital Center
- 2004–2005: Fellow, Stroke and Neurocritical Care, Massachusetts General Hospital (MGH)/Brigham and Women’s Hospital
- 2001–2004: Resident, Neurology, MGH/Brigham and Women’s Hospital
- 2000–2001: Intern, Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School
- 2000: Doctor of Medicine (MD), McGill University Faculty of Medicine
Honours (selected):
- 2022: Paper of the Month Award (JAMA Neurology publication), World Stroke Academy/World Stroke Organization
- 2018: Fellow, American Heart Association (FAHA)
- 2017, 2019–2023: Top Doctor, Boston Magazine
- 2012: Fellow, SVIN (FSVIN)
- 2004: Senior Neurology Resident Teacher of the Year Award, MGH/Brigham and Women’s Hospital