Results from the MSU-TELEMED randomised controlled trial—presented at the 11th European Stroke Organisation Conference (ESOC; 21–23 May, Helsinki, Finland)—have demonstrated that telemedicine-based neurologist assessments on mobile stroke units (MSUs) are more resource-efficient than traditional onboard neurologist models. Data also indicated that telemedicine-based MSUs were safe and did not significantly delay decision-making over stroke treatments.
“There’s been a longstanding assumption that having a neurologist physically onboard is the gold standard for MSU care,” said Vignan Yogendrakumar (University of Ottawa, Ottawa, Canada), principal investigator for the MSU-TELEMED trial. “But, our trial shows that telemedicine not only holds up—it delivers comparable outcomes in key operational domains.”
The trial was conducted across 10 tertiary hospitals in Melbourne, Australia, and is claimed by researchers to be the first prospective, head-to-head comparison of these two models of stroke care delivery. A total of 275 patients with suspected stroke were randomised based on the availability of onboard or telemedicine neurologist coverage.
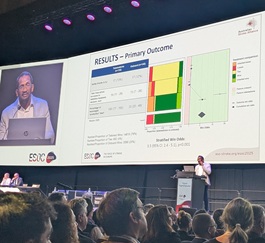
Using a novel, hierarchical, composite endpoint prioritising three distinct outcomes—safety, time to treatment decision, and resource utilisation—the study found that telemedicine significantly outperformed the onboard model, with 76% of patients’ outcomes favouring telemedicine compared to 21% for onboard care and 4% showing no difference. The stratified win odds ratio favouring the telemedicine model was 3.57 (95% confidence interval [CI], 2.4–5.2; p<0.0001).
Safety outcomes were also observed as being comparable between groups, with no significant difference in adverse event rates across patients allocated to telemedicine (12%) versus onboard (11%) models. The investigators further posit that, while the median scene-to-treatment decision time was four minutes longer in the telemedicine arm, this was offset by significantly lower resource usage, highlighting the model’s efficiency as compared to more traditional onboard approaches.
Another finding highlighted by the researchers is the fact that, among the 18% of patients who received intravenous thrombolysis (IVT) or were transported for endovascular therapy (EVT), no difference was observed in functional outcomes at 90 days—potentially underscoring telemedicine’s effectiveness even in high-stakes scenarios.
In the investigators’ view, the MSU-TELEMED trial’s results set a precedent for expanding tele-neurology services in prehospital stroke care, and may inform future deployment models that are both scalable and cost-effective.
Responding to an ESOC audience member’s question regarding the wider implications of these findings, Yogendrakumar noted: “We have shown, in concept, that you can have one neurologist covering a large area.”









