 From acute interventions to endovascular therapy indication expansion, Sunil Sheth from McGovern Medical School at UTHealth, Houston, USA, kick-started the Society of NeuroInterventional Surgery’s (SNIS) annual meeting (4–7 August) by outlining an array of recently completed, and ongoing stroke trials.
From acute interventions to endovascular therapy indication expansion, Sunil Sheth from McGovern Medical School at UTHealth, Houston, USA, kick-started the Society of NeuroInterventional Surgery’s (SNIS) annual meeting (4–7 August) by outlining an array of recently completed, and ongoing stroke trials.
“If I do not include your favourite trial, please forgive me,” he said. “Our goal today is to cover the full range of acute ischaemic stroke studies. From start to finish I will try to have representation from trials around the globe.”
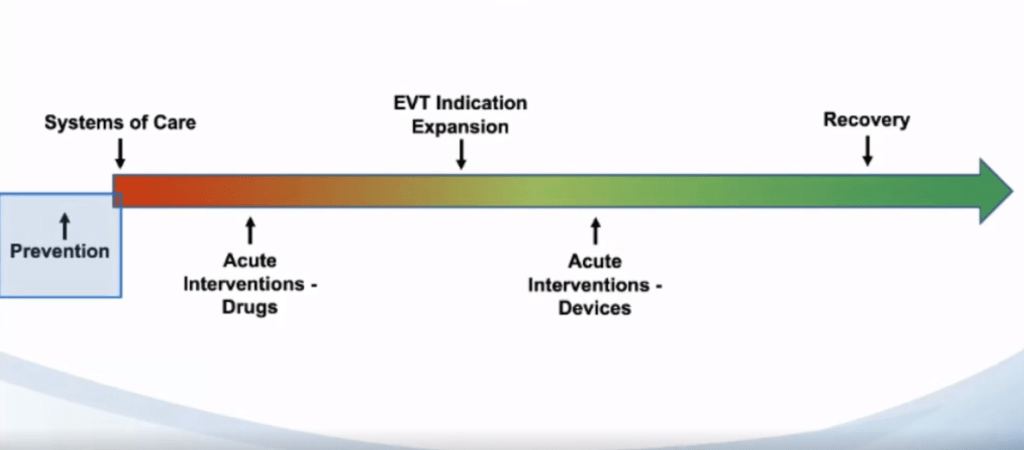
He explained to the audience that he has organised the trials by the segment of care; trials pertaining to prevention of stroke, systems of care, acute interventions, endovascular therapy indication expansion, and stroke recovery trials.
Prevention
The first trial Sheth alluded to was ARCADIA (Artrial cardiopathy and antithrombotic drugs in prevention after crypotogenic stroke). In this study, patients with embolic stroke of uncertain source (ESUS) are randomised to aspirin or apixaban. Sheth said it aims to answer the question: Which of these approaches is better at reducing the risk of subsequent or first-time stroke? The key criteria are ESUS, and evidence of atrial cardiopathy.
Next, he said that CREST2 (Carotid revascularisation and medical management for asymptomatic carotid stenosis trial)—a follow-up of CREST1—is investigating whether carotid revascularisation is, in fact, beneficial in preventing stroke. “The patients in this trial get randomised to either medical therapy or stenting endarterectomy. They have to have ≥70% stenosis and it has to be treatable. Like ARCADIA, this trial is enrolling, also with a target completion date of 2022,” Sheth explained.
Stroke systems of care
Pointing to trials pertaining to systems of care, he discussed the RACECAT trial—a prehospital stroke trial. “In Barcelona, Marc Ribo’s group is trying to answer the question: Which is the better routing strategy in the prehospital environment? Is it going from EMS directly to a primary stroke centre, or from EMS—bypassing the primary stroke centre—and going directly to a comprehensive stroke centre?
“The patients are being pre-screened and have to have some suspicion of LVO with a Rapid Arterial Occlusion Evaluation (RACE) score >4, and the trial is being conducted in areas where the local hospital cannot perform thrombectomy. This is a trial that is very closed to being completed, and I am looking forward to those results.”
The TRIAGE (Treatment strategy in acute ischemic large vessel stroke: prioritise thrombolysis or endovascular treatment) trial is similar, he said. In Denmark, patients are being randomised in the prehospital setting—either going directly to a primary stroke centre for IV tissue plasminogen activator (tPA) and then to a comprehensive stroke centre, versus going directly to the latter.
The last trial regarding optimising stroke systems of care he discussed was the BEST-MSU (Benefits of stroke treatment delivered using a mobile stroke unit) trial. Here, patients were randomised to either getting mobile stroke unit care versus standard EMS care, and had to be eligible for IV tPA. “They enrolled their last patient last week, so they are now completing their follow up and we should be hearing from them soon.”
Acute Interventions: Drugs
The next set of trials are interventional trials that involve medical therapies, Sheth told the SNIS online audience.
“The first is MOST (Multi-arm optimisation of stroke thrombolysis); a trial randomising patients that get IV tPA to receive either argatroban, eptifibatide, or placebo,” he said, adding that patients receive the study drug within one hour of IV tPA, and thrombectomy is allowed in these patients.
In addition, the TIMELESS (Tenecteplase in stroke patients between 4.5 and 24 hours) trial is randomising patients to either a single bolus dose of tenecteplase or placebo. Sheth noted that these patients are not IV tPA eligible, randomised between 4.5 to 24 hours of stroke onset. However, they have to have an LVO, and their imaging criteria must include a mismatch on CT perfusion and MRI. Like the MOST trial, TIMELESS is currently enrolling.
Sheth next introduced the first of several MR CLEAN follow-up trials. “MR CLEAN MED, a medical trial with a 2×2 factorial trial, includes patients with thrombectomy that was planned (with an LVO), getting randomised either to receive 300mg aspirin, or not, and/or a heparin bolus dose drip, or not. This is an open label study, so these are patients that are getting thrombectomy, with the drugs infused at the time of groin puncture, or right after IV tPA is completed.” He added that the study started in 2018, and is a third of the way through enrolment.
In terms of the MR CLEAN NO IV trial, Sheth told viewers that this explores the question of whether or not IV tPA is useful when patients are also getting thrombectomy. Key criteria include that patients must be IV tPA eligible (within 4.5hours), and have to have an LVO. “One of the unique aspects of this trial, like the original MR CLEAN trial, is that delayed consent is allowed, so you can screen and enroll, and randomise patients without consent upfront. Because of this, they have been enrolling very well; faster than expected, so the trial should be completed very soon,” Sheth highlighted.
Another trial looking to answer the same question is the SWIFT DIRECT (Bridging thrombolysis versus direct mechanical thrombectomy in acute ischaemic stroke) trial, which is randomising patients to thrombectomy (with Solitaire; Medtronic) with or without IV tPA. Again, these are IV tPA eligible patients with LVO, and an Alberta Stroke Program Early CT score (APECTS) ≥4. The estimated completion of this trial is 2022.
Endovascular therapy indication expansion
Sheth displayed the first set of four trials to the SNIS viewers, describing them as the “so-called large core trials”, which are exploring whether thrombectomy is helpful in patients that are presenting with an established moderate to large stroke. TESLA (Thrombectomy for emergent salvage of large anterior circulation ischaemic stroke) is testing thrombectomy versus medical management for patients with large cores (which is defined here as an ASPECTS 2–5 in patients up to 24 hours of stroke onset. In this study, internal carotid artery (ICA) or M1 occlusions are allowed, but tandem occlusions are being avoided. Currently over 40/300 patients have been enrolled.
“Then we have the TENSION trial out of Europe, which again explores thrombectomy versus medical management for large core,” Sheth explains. However, while the study has similar inclusion criteria to TESLA, large core is defined as ASPECTS 3–5. Sheth said it has a larger sample size (n=655), with around 93 patients enrolled so far.
Regarding the remaining large core trials, Sheth said the LASTE (Large stroke therapy evaluation–ASPECTS 0–5) trial, part of the IN EXTREMIS cohort, defines large core as ASPECTS 0–5, up to 6.5 hours after stroke onset, and also includes ICA or M1 occlusions, while the SELECT 2 trial is similar, but a “major difference” is that CT perfusion is required in these patients.
“At the opposite end of the spectrum, we have the low National Institutes of Health Stroke Scale [NIHSS] studies,” Sheth said.
First, he introduced the ENDOLOW (Endovascular therapy for low NIHSS ischaemic strokes) trial, which examines thrombectomy (with Embotrap; Cerenovus) versus medical management (with possible thrombectomy rescue) in patients with ICA or M1 occlusions that have an NIHSS score 0–5. “Imaging criteria for this trial is ASPECTS ≥6,” Sheth added, “and there are also some CT perfusion and MRI criteria as well. The trial is currently enrolling, estimated to be completed by next year.”
According to Sheth, the MOSTE (Minor stroke therapy evaluation—NIHSS 0–5) trial is also looking into thrombectomy versus medical management, with possible thrombectomy rescue within 24 hours, with ASPECTS screening as an inclusion requirement.
“In terms of the EVT indication expansion trials, we also have a Chinese endovascular trial (BAOCHE), investigating whether or not basilar artery occlusion patients benefit from thrombectomy, which is still an outstanding question, at least from a clinical trial point of view,” he told the SNIS audience.
Lastly, he explained that the MR CLEAN LATE trial is a late time window trial. He proposed that it is different from DAWN and DEFUSE 3 as CT perfusion is not required. Instead, the imaging requirement is CTA collateral grading.
Acute interventions: Devices
Next, Sheth alluded to a number of studies looking at devices, which are mostly industry-sponsored. The EXCELLENT trial, sponsored by Cerenovus, is studying the Embotrap through a prospective registry. The COMPLETE study is looking at the Penumbra aspiration catheters and the 3D separator. Sheth said this trial is now complete, and the results should be out soon. PROST by Phenox is looking at their Preset device versus the Solitaire (Medtronic) device. “This is not a registry,” Sheth explained, “but a randomised trial between two treatment approaches.”
The TIGER trial that Rapid Medical has recently completed investigated their Tigertriever as a prospective study. According to Sheth, Imperative Care’s trial is coming soon, which seeks to compare their Zoom aspiration catheters to Solitaire or Trevo (Stryker). Finally, he said the INSIGHT study by Penumbra is a registry for thrombus collection in thrombectomy and intracerebral haemorrhage evacuation. “But this is not a device trial, per se,” he added.
Stroke recovery trials
“There is a whole suite of recovery trials, but I am going to focus on two,” Sheth told the audience. PISCES III (Investigation of neural stem cells in ischaemic stroke) involves testing a stereotactic injection of stem cells into a region adjacent to the infarct, versus sham surgery. Key criteria for this, according to Sheth, include some residual arm function, stroke within six to 24 months, and sufficient language function. Enrolment for PISCES III is complete.
The concluding trial of his talk referred to one examining transcranial direct current stimulation (tDCS) and task-specific practice for post-stroke neglect. The design involves comparing bilateral parietal tDCS versus bilateral primary motor cortex tDCS, versus sham plus task-specific practice. In terms of its status, Sheth said it is still enrolling.
For more stories from SNIS 2020, click here.