Important methodological aspects of clinical trials of spinal cord stimulation (SCS) using a placebo are consistently being poorly reported, says a recent systematic review. Within the context of the fast-evolving field that is neuromodulation, the authors, Rui V Duarte from Liverpool Reviews and Implementation Group (University of Liverpool, Liverpool, UK) and colleagues’ express concern about the validity and replicability of the current literature.
Within their appraisal, published in Neuromodulation, Duarte et al allude to the important aspects that need to be clearly reported, including the reporting of stimulation programming parameters, patient position during perception threshold measurement, management of the patient handheld programmer, frequency of recharging, as well as the assessment of the fidelity of blinding.
Throughout the medical literature, high-quality randomised controlled trials (RCTs) are considered to be the “gold standard” to evaluate the effectiveness of a treatment. Yet, the authors acknowledge that “in contrast to drug therapies, providing an appropriate placebo control in clinical trials of healthcare procedures involving a medical device is often much more challenging.” Nevertheless, Duarte and colleagues point to the advent of a new “comparator arm” for RCTs to investigate the effectiveness of SCS. Despite blinding difficulties, they write that a number of small studies have managed to compare conventional or paraesthesia producing SCS to sham stimulation.
Thus, by systematically reviewing the current evidence base of RCTs regarding SCS placebo/sham trials alongside critiquing the corresponding literature, Duarte and his team developed a checklist for the design and reporting of future RCTs.
In order to carry out this task, they searched electronic databases from inception until January 2019, while any RCTs that included only an active comparator were excluded. Ultimately, 12 eligible RCTs were identified. The modalities that were assessed included: paraesthesia stimulation, subthreshold, burst and high-frequency SCS, which were predominantly conducted on patients with failed back surgery syndrome, complex regional pain syndrome, and refractory angina.
The authors write, “The quality and transparency of reporting of the methods of placebo stimulation, blinding of patients, clinicians, and researchers varied markedly across studies. In the 12 RCTs identified in this systematic review, the placebo varied from simply switching off the SCS device to more complex approaches such as intermittent switch on of low current stimulation or programming a current leak during the placebo periods so that the recharging time and frequency were equivalent during the different crossover periods.”
In light of such shortcomings, Duarte et al propose that authors of future SCS placebo-controlled studies should consider a number of specific aspects of the design and reporting of any subsequent trials.
Regarding studies using non-rechargeable devices, the authors point to the importance of programming parameters for the active and sham arm, as well as how the patient handheld programmer is managed and, if a handheld programmer is provided to the patients, to think about how blinding is ensured. For studies utilising subthreshold programming as a comparator, Duarte and colleagues note that these investigations should “specify the position(s) in which the threshold was measured in and whether a feedback loop/position adjustment was utilised to modulate current intensity”.
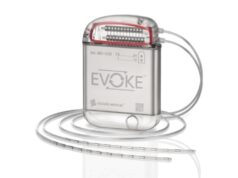
In terms of rechargeable devices, the authors maintain that the use of a placebo is further compounded by a number of factors, including the need for the patients in both arms to experience a similar recharging burden. “Accordingly,” they add, “the frequency and duration of recharging should be reported. This is important in both cross-over and parallel design studies.”
In addition, they emphasise that the management of both patient handheld programmers and patient rechargers needs to be specified. And, for the latter, particularly where the recharger contains a feedback screen that allows the subject to assess IPG (implantable pulse generator) charge.
“There are several possibilities to manage sensations related to placebo responses depending on the nature of the active comparator. These include devices that cyclically switch on to deliver a short burst of suprathreshold stimulation, devices that deliver subthreshold current of very low intensity continuously or intermittently [and] devices that are fully switched off,” write the authors. Yet they highlight, “Only this [latter] strategy avoids the risk that stimulation might be therapeutic, even when the dose is minimal. Use of a full switch off strategy against a paraesthesia stimulation comparator risks unblinding participants.”