 A recent study demonstrates the potential value of percutaneous peripheral nerve stimulation (PNS) for chronic low back pain. Data reported by Christopher A. Gilmore and colleagues, Center for Clinical Research, Carolinas Pain Institute, Winston Salem, USA, published in the journal of Neuromodulation, found that improvements in pain, medication, as well as patient-centric outcomes, lasted beyond the removal of percutaneous PNS leads.
A recent study demonstrates the potential value of percutaneous peripheral nerve stimulation (PNS) for chronic low back pain. Data reported by Christopher A. Gilmore and colleagues, Center for Clinical Research, Carolinas Pain Institute, Winston Salem, USA, published in the journal of Neuromodulation, found that improvements in pain, medication, as well as patient-centric outcomes, lasted beyond the removal of percutaneous PNS leads.
Although a prescribing physician may find it difficult to escape the press surrounding the opioid epidemic, Gilmore and colleagues shed light on the current crisis, writing: “Neuromodulation may provide an opportunity to reduce the need for opioids for chronic LBP”, and acknowledged that so far, “the cost and invasiveness of existing systems have limited its adoption”.
Initially designed to enable percutaneous delivery of therapy without surgery while reducing complications, the authors put forward that “percutaneous PNS also provides a less-invasive and less costly treatment option to reduce pain and disability”.
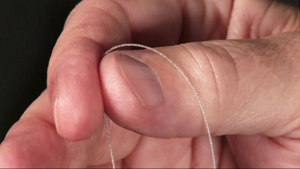
The SPRINT PNS system (SPR Therapeutics, Inc., Cleveland, OH) features a lead with a 100-micron coiled wire design (see image, courtesy SPR Therapeutics) intended to reduce lead migration that has demonstrated a very low risk of infection. “If successful, this approach has the potential to provide effective neuromodulation therapy earlier in the treatment continuum,” Gilmore et al writes.
To evaluate the use of percutaneous PNS for the treatment of chronic low back pain (LBP), patients with chronic LBP were enrolled in an FDA investigational device exemption case series. Specifically, subjects with chronic axial LBP—pain confined to the lumbar region, lasting at least 12 weeks—were eligible for participation. Percutaneous PNS leads targeted the medial branch of the dorsal ramus in the region of the LBP. These fine-wire leads were implanted using ultrasound-guidance and known anatomical landmarks and remained in place for the 30-day therapy.
In total, nine subjects (mean age: 53.5 years) met the criteria. Subjects reported an average pain intensity (BPI-5) of 5.7 and a worst pain intensity (BPI-3) of 7.7 at baseline. Following PNS treatment, the majority of these subjects reported statistically and clinically significant reductions in both average pain intensity (BPI-5; average reduction of 3.4) and worst pain intensity (BPI-3; average reduction of 4.4) scores, which continued through to the four-month follow-up. In addition, subject-reported reductions in pain intensity were demonstrated by concomitant and sustained reductions in analgesic medication use, while clinically significant reductions in patient-centric outcomes of disability, pain interference and patient global impression of change were also reported by subjects.
Thus, these improvements in pain, medication use, and patient-centric outcomes led Gilmore and colleagues to conclude that the current study demonstrates the potential value of percutaneous PNS for the treatment of chronic LBP.
On further discussion of the findings, the authors maintain that the therapy outlined in the current study holds the potential to shift the paradigm surrounding chronic pain management. “Along with providing the benefits of neuromodulation therapy to patients early in the treatment continuum […], the present work highlights the value and safety profile of this approach.”









