Following the introduction of its BrainPath navigation probe adapter at the International Stroke Conference (ISC 2022; 9–11 February, New Orleans, USA), medical device innovator NICO Corporation claims to have become the first and only provider to offer an adapter for electromagnetic navigation (EM) when performing minimally invasive parafascicular surgery—giving neurosurgeons the option to deploy a frameless brain surgery procedure.
This means, according to a NICO press release, that appropriate patients will no longer have to be pinned in a rigid headframe during the navigation process, providing a more compassionate, minimally invasive surgery option.
The BrainPath navigation probe adapter for the Medtronic StealthStation EM is used with specific navigation pointers during minimally invasive parafascicular surgery procedures. This technology further differentiates NICO’s platform solution to provide surgeons more choices and efficiencies in the operating room based on what is needed for each patient, the release adds.
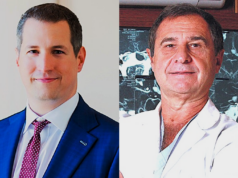
“The simple and easy operating room setup with frameless stereotaxy and BrainPath helps us get the patient treated in a safe, fast and efficient way,” said Justin Singer (Spectrum Health, Grand Rapids, USA). “I have found this to be a great option for patients where pinning would not be indicated for subcortical tumour removal and beneficial in treating emergent haemorrhagic stroke patients.”
The BrainPath adapter is a sterile, single-use accessory that secures the position of the EM pointer during BrainPath cannulation. It is part of an integrated platform system for brain surgery that NICO claims “did not previously exist”—providing safe subcortical access to all regions of the brain, automated removal of brain abnormalities, and simultaneous biological preservation of collected tissue for use in the delivery of novel therapeutics and potential implantation to the brain.
In its limited market evaluations, involving more than 20 cases, surgeons reported the navigation probe adapter as “ideal” for emergent intracerebral haemorrhages (ICH), traumatic ICH and subcortical tumours, citing seamless integration in the operating room and workflow efficiencies, the release also notes.