Two data analyses presented at the recent Society of NeuroInterventional Surgery (SNIS) annual meeting (22–26 July, Colorado Springs, USA) have revealed new insights on the role of rescue stenting following failed mechanical thrombectomy, with one indicating parity between different stent types and the other suggesting that the approach holds minimal benefits compared to medical management in these cases.
During a late-breaking abstract session at SNIS 2024, Mahmoud Mohammaden (Emory University, Atlanta, USA) presented a post-hoc analysis of the SAINT study—a multicentre collaboration involving prospectively collected databases that was published last year and concluded that rescue stenting results in better functional outcomes as well as a comparable safety profile versus procedure termination after failed thrombectomy in both anterior- and posterior-circulation stroke patients.
The analysis delivered by Mohammaden used data from SAINT to specifically compare balloon-mounted versus self-expandable stenting approaches, with 329 patients enrolled consecutively across 15 comprehensive stroke centres in the USA meeting its inclusion criteria. Overall, there were 125 patients treated with a balloon-mounted stent—including 56.8% with drug-eluting stents and 39.2% with bare-metal stents—and 204 treated with a self-expandable stent, most commonly Enterprise (Cerenovus/J&J), Wingspan or Neuroform Atlas (both Stryker).
The investigators determined that the balloon-mounted and self-expandable stenting groups were well-balanced in terms of baseline clinical and procedural characteristics.
“Interestingly, there was no difference in the procedure duration between both groups,” Mohammaden relayed, “and, also, there was no difference in terms of balloon angioplasty—reflecting the fact that ‘newer’ interventionists tend to use balloon angioplasty for stenting to avoid long-term antiplatelet use.”
Arriving at the analysis’ primary endpoint finding—successful final reperfusion defined as modified thrombolysis in cerebral infarction (mTICI) ≥2b—the presenter noted that balloon-mounted stenting was associated with increased likelihood of achieving a higher degree of reperfusion on the mTICI scale compared to self-expandable stenting (adjusted common odds ratio [aOR], 2.2; p=0.003), as well as higher rates of mTICI ≥2 reperfusion (aOR, 6.17; p=0.001).
However, these improved technical outcomes did not translate into better clinical results, as 90-day modified Rankin scale (mRS) shift findings, and rates of mRS 0–2 and 0–3, were all statistically similar between the two groups. In parallel, the rates of procedural complications, symptomatic intracranial haemorrhage (sICH) and mortality were ultimately comparable between groups too.
The investigators also determined that there was no treatment-effect modification of stent type on the final reperfusion grade or mRS score shifts across the study’s prespecified subgroups—including age, stroke aetiology and occlusion site.
“In conclusion, in patients who failed mechanical thrombectomy and underwent rescue stenting, our study showed that balloon-mounted stents had higher rates of reperfusion compared to self-expandable stents,” Mohammaden noted. “However, the likelihood of disability, and good and fair outcomes as well as the safety measures, were comparable in both groups.”
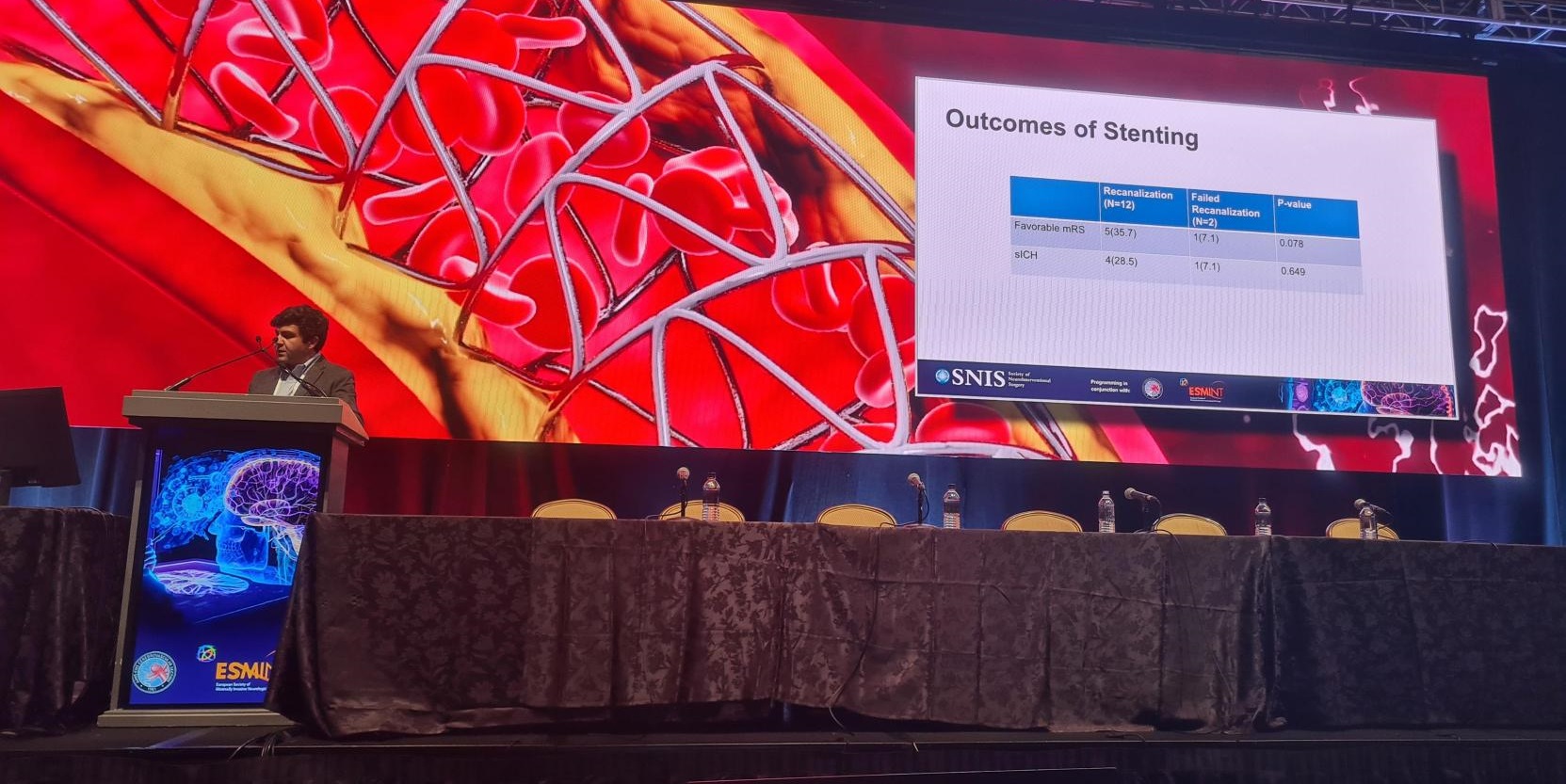
A similar topic was the focus of the late-breaking session’s next talk, with multicentre findings on the safety and efficacy of post-thrombectomy rescue stenting being presented by Kasra Khatibi (University of Southern California, Los Angeles, USA) on behalf of Humain Baharvahdat (Rothschild Foundation Hospital, Paris, France) and colleagues.
Via a retrospective cohort study conducted between 2012–2024, investigators compared rescue stenting to medical management after a failed thrombectomy procedure, with failure being defined as TICI ≤2a reperfusion. Their primary endpoint was good functional outcome, quantified by an mRS score of 0–2, with postprocedural sICH being among key secondary endpoints.
Of 89 patients who underwent a failed thrombectomy throughout the specified timeframe, 30 received rescue therapy with stenting or angioplasty, while the remaining 59 received maximal medical management. Some 37% of these patients subsequently achieved TICI ≥2b reperfusion. The investigators extracted two well-matched, comparable groups from this cohort—one of which included 14 patients who underwent rescue stenting and another that included 14 patients who received medical management—for further analysis.
Baharvahdat and colleagues’ functional outcome results ultimately revealed statistical parity between these groups, although they did find a trend towards a higher rate of mRS 0–2 at discharge in the medical management group (71.4%) versus the rescue stenting group (42.8%). Mortality rates were identical between the two groups, with four deaths occurring in each, and occurrence of sICH was also statistically similar (rescue stenting, 35.8% vs medical management, 42.8%). Additionally, the investigators noted a significantly higher rate of decompressive hemicraniectomy procedures in those who received medical management (42.8%) compared to rescue stenting (0%).
They therefore concluded that—while antithrombotic therapies were not found to have led to an increase in bleeding-related complications—rescue stenting was not associated with a meaningful alteration of post-thrombectomy clinical outcomes, as compared to medical management.
Finally, a subanalysis of Baharvahdat and colleagues’ rescue stenting group revealed that patients who achieved successful reperfusion (TICI ≥2b) were more likely to experience favourable functional outcomes (mRS 0–2), but more likely to suffer sICH as well.