This advertorial, sponsored by Siemens Healthineers and intended for US readers only, is part of a series of articles on the emerging role for neurovascular office-based labs (OBLs).
Neurovascular diseases present formidable obstacles for both patients and healthcare providers. As advancements continue to unfold within the realm of neurovascular intervention, the emergence of OBLs is progressively reshaping the delivery of specialised care, offering innovative solutions to these longstanding challenges.
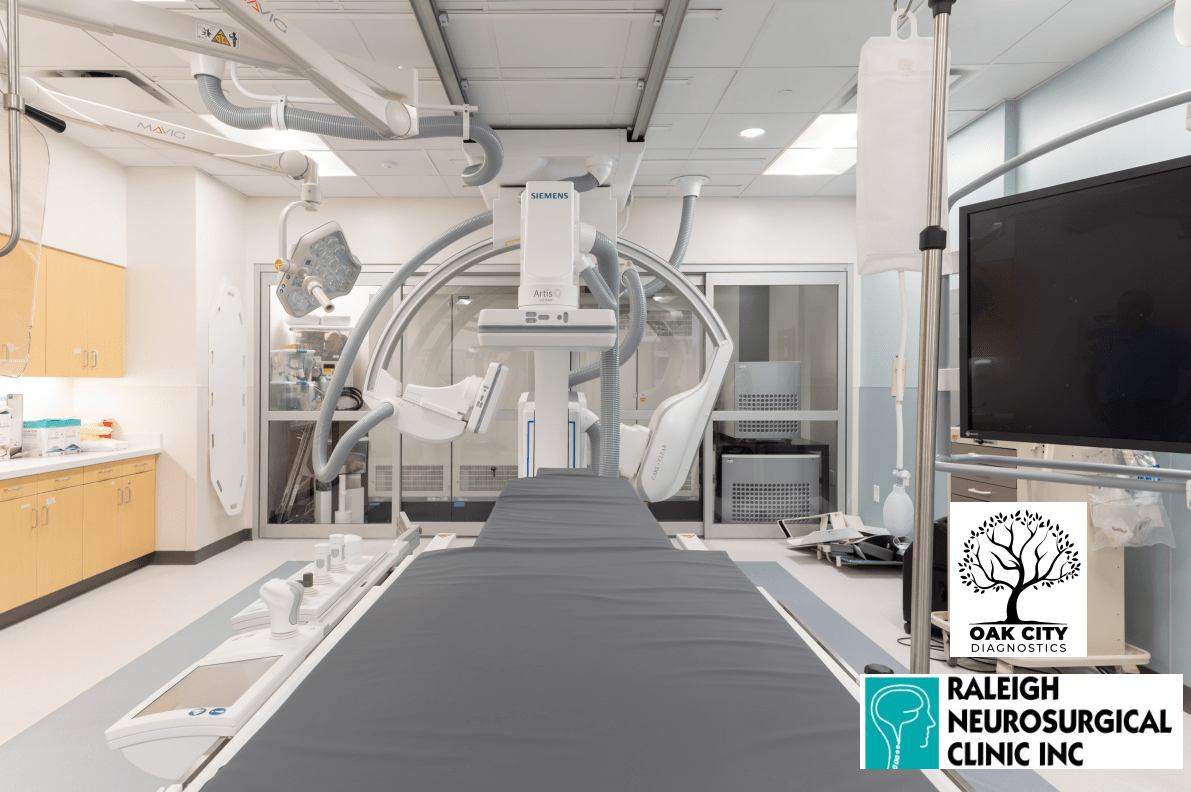
In our previous edition, the leading practitioners at Raleigh Neurosurgical Clinic in Raleigh, USA shared their pioneering journey. They unveiled their transformation as the inaugural office-based neuroendovascular practice nationwide to incorporate a Siemens Healthineers fixed biplane angiography system.
In the following discourse, they delve deeper into the intricate dynamics between an OBL’s impact on patient outcomes and an evolving reimbursement landscape. Together, these factors forge a compelling business case for the modernisation of neurovascular care delivery.
Improved patient outcomes
Raleigh Neurosurgical Clinic is swiftly gaining a reputation for its innovative approach to patient care, particularly for conditions such as stroke, aneurysms, and arteriovenous malformations. This private practice harmoniously integrates advanced technology, expert care, and personalised service, all situated within the comfortable and accessible framework of an outpatient setting.
Andrey Belayev, a neuroendovascular surgeon at the clinic, elaborates on their operating strategy: “We perform diagnostic angiography and straightforward procedures at our OBL, reserving the hospital environment for more complex interventions. Approximately 99% of our OBL procedures consist of diagnostic cerebral angiography—a technique involving endovascular catheterisation and brain imaging. We also conduct spinal angiography and kyphoplasty procedures. Our use of the Siemens Healthineers biplane angiography system sets us apart from many OBLs that operate with single plane angiography systems. This superior technology enables us to acquire double the data or imaging compared to a single plane system, thereby accelerating the procedure and decreasing the risk to the patient.
“In the hospital, we rely on the femoral approach, because procedures are more complicated or complex and often require the use of other devices. It is a different scenario there. Furthermore, hospital recovery nurses typically take care of many patients, so they do not always have the time or proximity to offer individual attention. Patients are spread out, and the level of attention they receive in our OBL setting is not always possible.”
He further emphasises the efficiency of their OBL procedures, stating: “By performing our angiograms using a radial approach, patients can mobilise more quickly and recovery time is reduced to just two hours. This heightens patient comfort and contributes to a more efficient experience.”
The OBL model places a high emphasis on convenience and accessibility, providing a less intimidating environment for patients to receive their treatment. This can significantly lower anxiety and enhance overall patient satisfaction. Additionally, OBLs typically offer shorter wait times for procedures, enabling more timely interventions and potentially leading to improved clinical outcomes.
Jacob Rodman, the clinic’s chief executive officer (CEO), compares the patient experience at their clinic to a boutique service.
“We provide patients with iPads to stream entertainment,” he says. “They can catch up on the news, or enjoy a snack and refreshments, in a relaxed setting. Our primary concern is ensuring that the right care is delivered in the right place. This approach not only benefits our patients but also allows hospital angio suites to focus on caring for more critically ill individuals.”
The adaptability inherent in the OBL model allows for the selection of the most suitable technology and equipment for minimally invasive procedures too. The clinic’s use of the Siemens Healthineers biplane angiography system exemplifies this advantage. By minimising the physical and emotional stress often associated with traditional, hospital-based care, OBLs like Raleigh Neurosurgical Clinic are significantly contributing to enhancing patient outcomes and the overall quality of life.
Business outcomes
Neurovascular OBLs offer significant business benefits for healthcare providers, presenting a pathway to enhance operational efficiency, bolster cost-effectiveness, and amplify financial performance.
Operating with a streamlined workflow and specialised staff, OBLs facilitate efficient patient throughput and diminished overhead costs. By homing in on neurovascular interventions, OBLs can leverage economies of scale, channel investments into cutting-edge equipment, and attract top-tier neurointerventional specialists. This concentration of expertise often culminates in superior clinical outcomes, thus solidifying OBLs as favoured destinations for both patients and referring physicians.
Moreover, the business model of OBLs fosters predictable and steady revenue streams. With a strategic focus on specialised procedures, OBLs have the ability to negotiate advantageous reimbursement contracts with payers, which effectively mitigates financial uncertainties. The industry-wide shift towards value-based care and bundled payments further incentivises OBLs to optimise outcomes while conscientiously managing costs, thereby fostering financial stability and growth.
Expanding on the business advantages, OBLs’ streamlined processes and shorter wait times can result in an enhanced reputation—not only among patients but also within the larger healthcare community. This can attract additional referrals, further boosting revenue and growth potential. A reputation for high-quality, efficient care can also attract more skilled professionals to the OBL, further contributing to its clinical and financial success.
Additionally, OBLs can be more agile and innovative compared to larger, more bureaucratic hospital systems. This agility allows for rapid adoption of emerging technologies and techniques, which can further enhance patient outcomes, operational efficiency and cost-effectiveness. Thus, by being at the forefront of neurovascular care, OBLs can better negotiate with vendors, ensuring they secure the best possible terms and maintain their competitive edge in this rapidly evolving field.
Reimbursement trends
Reimbursement is a pivotal component in ensuring the sustainability and expansion of neurovascular OBLs. Grasping the evolving reimbursement landscape is crucial for navigating the intricacies of billing processes and guaranteeing fair compensation for services rendered.
The value added by OBLs in the realm of neurovascular care is increasingly being recognised. Payers are progressively acknowledging the cost-effectiveness and superior outcomes demonstrated by these facilities, leading to wider coverage for procedures performed within an OBL setting.
Humorously, Belayev notes: “You do not get paid more for delivering tomorrow’s care today. However, payers are advocating for a higher number of procedures to be performed in outpatient settings. We have witnessed this transition over the years. We are now performing more complex spine surgeries in the ASC [ambulatory surgery centre] setting. Anticipating and responding to that need early on was the optimal strategy for our private practice.
The shift towards value-based reimbursement models underscores the importance of patient outcomes and quality metrics. OBLs that consistently demonstrate excellent clinical outcomes and high levels of patient satisfaction may negotiate higher reimbursement rates and secure partnerships with accountable care organisations (ACOs), and other risk-sharing entities.
“Until changes in coding and reimbursement are implemented through Medicare and private payers, we are somewhat restricted in what we can achieve,” Belayev adds. “At present, we face challenges in integrating interventions into the OBL setting. However, payers are eager for this transition, and it is not going to impede the emergence of OBLs. I am confident that changes in payment policies will align with this evolving model.”
It is crucial for OBLs to stay informed about changes in reimbursement policies, ensure accurate documentation, and actively participate in quality improvement initiatives. Collaborative efforts with professional societies, advocacy for fair reimbursement and lobbying are all key to securing the long-term viability of neurovascular OBLs.
Conclusion
Neurovascular OBLs have emerged as a transformative force in the field of neurointerventional care. By prioritising patient outcomes, optimising business performance, and rapidly adapting to the evolving trends in reimbursement, OBLs are uniquely positioned to deliver high-quality, cost-effective care for patients with neurovascular diseases.
As the healthcare landscape continues to evolve, it is crucial for OBLs to stay proactive, embrace new technologies, adjust to regulatory changes, and keep up with evolving reimbursement models, ensuring their sustained success in improving patient outcomes and shaping the future of neurovascular care.
Belayev predicts: “I foresee a rise in the number of neurovascular OBLs in the future, following a similar model. We may be among the first, but this idea has been under consideration for some time. This is just the beginning.”
Click here to learn more about fixed neuro angiography systems for OBLs. This is Part 2 of an OBL series highlighting the benefits for neurovascular procedures—click here to read Part 1 of the series.
 Andrey Belayev, an endovascular neurosurgeon at Raleigh Neurosurgical Center (Raleigh, USA), is board certified in neurosurgery. In addition to his clinical practice as a general neurosurgeon, he specialises in the treatment of neurovascular disorders including aneurysms, vascular malformations of the brain and spine, carotid artery stenosis, and the acute treatment of stroke. Belayev earned his medical degree at the University of Miami Miller School of Medicine (Miami, USA). He then completed his residency in neurosurgery at the University of Texas Health Science Center at San Antonio (San Antonio, USA), where he served as chief resident. He completed his fellowship training in open cerebrovascular surgery and endovascular neurosurgery at the prestigious Semmes-Murphey Clinic (Memphis, USA), and completed a fellowship and advanced clinical training in microvascular and endovascular neurosurgery with the World Federation of Neurological Societies in Nagoya, Japan. Belayev is the author of several peer-reviewed manuscripts and has been invited to present his research findings at respected clinical meetings around the world.
Andrey Belayev, an endovascular neurosurgeon at Raleigh Neurosurgical Center (Raleigh, USA), is board certified in neurosurgery. In addition to his clinical practice as a general neurosurgeon, he specialises in the treatment of neurovascular disorders including aneurysms, vascular malformations of the brain and spine, carotid artery stenosis, and the acute treatment of stroke. Belayev earned his medical degree at the University of Miami Miller School of Medicine (Miami, USA). He then completed his residency in neurosurgery at the University of Texas Health Science Center at San Antonio (San Antonio, USA), where he served as chief resident. He completed his fellowship training in open cerebrovascular surgery and endovascular neurosurgery at the prestigious Semmes-Murphey Clinic (Memphis, USA), and completed a fellowship and advanced clinical training in microvascular and endovascular neurosurgery with the World Federation of Neurological Societies in Nagoya, Japan. Belayev is the author of several peer-reviewed manuscripts and has been invited to present his research findings at respected clinical meetings around the world.
 Jacob Rodman is the CEO for Raleigh Neurosurgical Clinic—a group that was established in 1954. Rodman has over 20 years of management experience encompassing leadership positions at every level. He is a past president and board member for the North Carolina Medical Group Managers Association (NCMGMA). He has also served on several advisory committees and boards for United Healthcare of North Carolina, Blue Cross and Blue Shield of North Carolina, the Town of Morrisville’s budget office, Medical Mutual Insurance Company, and Wake Monarch Academy. Rodman is currently president elect for the Neurosurgery Executive Resource Value and Education Society (NERVES). He is also a board-certified medical practice executive by the American College of Medical Practice Executives (ACMPE), and has presented both nationally and internationally on a variety of topics surrounding medical practice management and leadership.
Jacob Rodman is the CEO for Raleigh Neurosurgical Clinic—a group that was established in 1954. Rodman has over 20 years of management experience encompassing leadership positions at every level. He is a past president and board member for the North Carolina Medical Group Managers Association (NCMGMA). He has also served on several advisory committees and boards for United Healthcare of North Carolina, Blue Cross and Blue Shield of North Carolina, the Town of Morrisville’s budget office, Medical Mutual Insurance Company, and Wake Monarch Academy. Rodman is currently president elect for the Neurosurgery Executive Resource Value and Education Society (NERVES). He is also a board-certified medical practice executive by the American College of Medical Practice Executives (ACMPE), and has presented both nationally and internationally on a variety of topics surrounding medical practice management and leadership.
Disclaimer: The statements by Siemens Healthineers’ customers described herein are based on results that were achieved in the customer’s unique setting. Since there is no “typical” hospital and many variables exist (e.g. hospital size, case mix, level of IT adoption), there can be no guarantee that other customers will achieve the same results.