Middle meningeal artery (MMA) embolisation—the injection of a liquid embolic substance to block an artery feeding the brain’s dura—along with surgery for subacute or chronic subdural haematoma (SDH) has been found to reduce the risk of patients requiring repeat surgery, as compared to surgical drainage alone, in the EMBOLISE clinical trial. This finding was delivered at the International Stroke Conference (ISC; 7–9 February, Phoenix, USA) within a preliminary late-breaking science session.
“The EMBOLISE trial showed that there was a nearly three-fold reduction in reoperation for patients that were treated with surgery plus embolisation,” said study co-author Jason Davies (State University of New York, Buffalo, USA), who presented the results of EMBOLISE earlier today alongside Jared Knopman (Weill Cornell Medical College, New York, USA). “Fewer trips to the operating room mean less potential for pain, complications, recovery and expense for the patient. Furthermore, we see that the complications related to the embolisation procedure were low and that there was no increase in neurological problems.”
While many SDHs occur because of physical trauma sustained following, for example, a car accident or violent fall involving head injuries, a subacute SDH generally occurs following less severe trauma—such as a concussion—with symptoms including weakness, numbness, tingling, seizure, headache, confusion or dizziness developing over the course of several hours or days after the event. And, according to a recent American Heart Association (AHA) press release, chronic SDH can result from slow bleeding after minimal trauma that the patient “may not even remember”, with symptoms potentially being subtle and/or taking weeks to be noticeable enough for them to seek treatment.
“Chronic subdural haematoma is one of the most common neurosurgical conditions and is likely to increase in the future since we have a sizeable ageing population, with many taking blood thinners to manage various medical conditions,” Davies continued. “These haematomas often form in the elderly because, as we age, the brain shrinks and pulls away from the inside of the skull, stretching the veins that form a bridge between the dura and the brain, which makes them more likely to tear after a small trauma and leak blood into the protective space between the brain and skull—the dura.”
Standard treatment for subacute or chronic SDH may involve a surgical procedure to drain pooled blood from the area, or the close monitoring of symptoms to determine if and when intervention may be necessary. The challenge here is that, even after surgery, repeat procedures may be needed in up to 20% of SDH cases, according to the AHA.
The EMBOLISE study explored the additive treatment option of MMA embolisation for subacute or chronic SDH—specifically testing whether these cases are likely to require additional surgery if, in addition to surgical drainage, a substance is injected to embolise one of the arteries supplying blood to the dura. The substance used in the trial, the Onyx liquid embolic system (Medtronic), is already used prior to surgery to reduce bleeding in people having an operation to correct an abnormal connection between arteries and veins in the brain known as arteriovenous malformations (AVMs). Onyx works by starting out as an injectable soft solid, before flowing as a liquid when force is applied, and then returning to a soft solid state post-injection to stop the blood vessel leaking.
Between December 2020 and August 2023, EMBOLISE researchers enrolled 400 adults (average age, 72 years; 27% women) across 39 US centres including both community and academic hospitals. All were about to undergo surgery for subacute or chronic SDH, and were considered able to care for themselves and likely to survive for at least one year. Patients were randomly assigned to receive either surgery alone or surgery plus MMA embolisation using Onyx to help reduce the progression or recurrence of their SDH. EMBOLISE’s primary outcome was how frequently there was reaccumulation of blood i.e. a recurrence of SDH that required surgical drainage within 90 days.
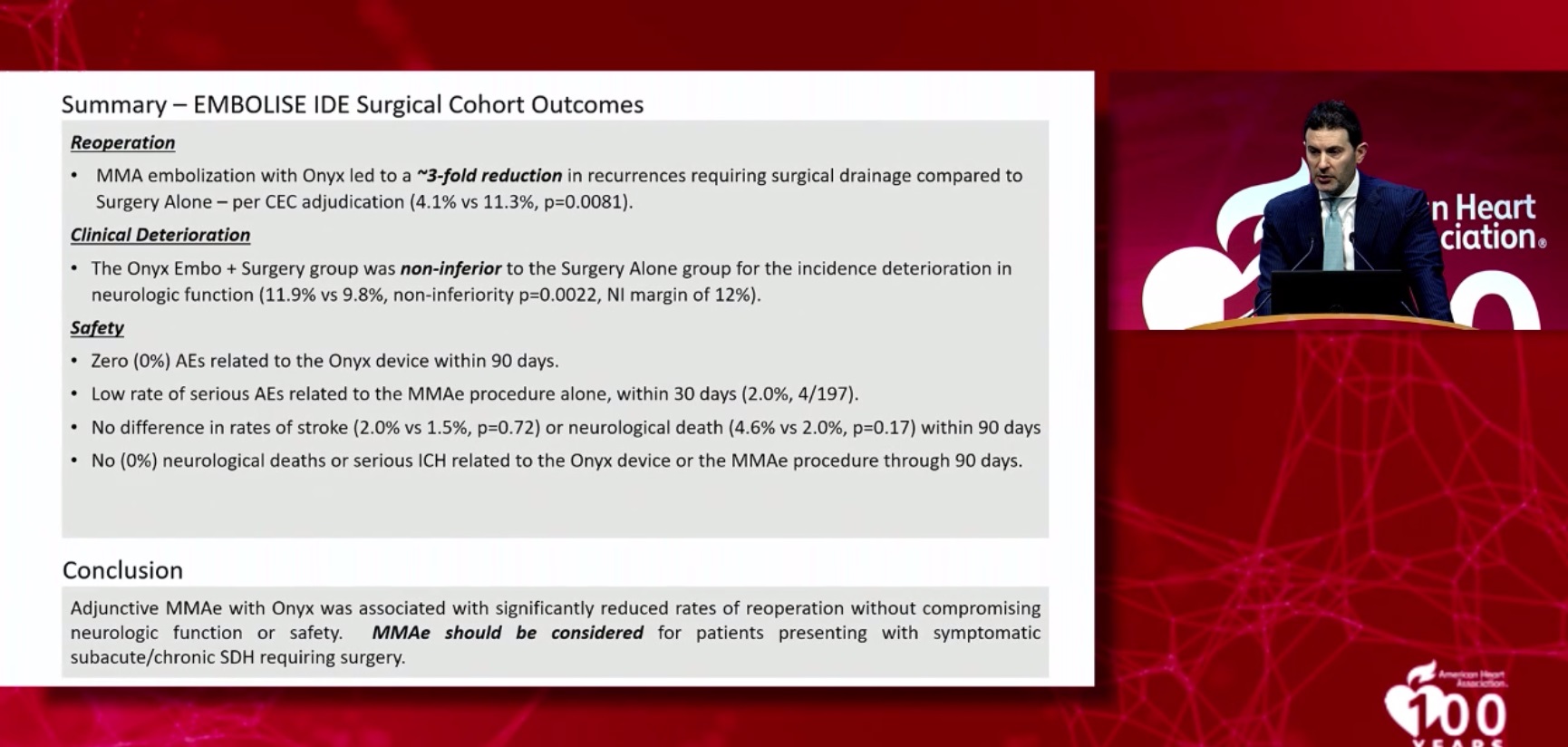
Key findings from the study are as follows:
- Subsequent SDH within 90 days and need for surgical drainage was observed in 4.1% of patients who had surgery plus embolisation compared to 11.3% in those who had surgery alone
- At 90 days after surgery, increasing disability and neurological dysfunction was found to be statistically comparable between the two treatment groups, occurring in 11.9% of patients who had surgery plus embolisation and 9.8% of patients who had surgery alone
- Serious adverse events attributed to MMA embolisation occurred in 2% of patients who received it
Additional measures to gauge the effectiveness of the liquid embolic treatment included the number of hospital readmissions; change in haematoma volume or thickness; and change in midline shift, whereby a haematoma pushes brain tissue out of alignment. All of these outcomes were assessed at 90 days after treatment, but were not presented at ISC 2024. Other arms of the EMBOLISE study—which included patients not undergoing surgery, who were randomised to either receive the liquid embolic system or not—are ongoing, and were not presented at ISC either.
The main limitation in this analysis of the study, according to Davies, was a relatively high loss to follow-up.
“One of the challenges of conducting this trial was dealing with a frail, elderly population, especially in the middle of the pandemic,” he noted. “Tracking patients down for follow-up is always a challenge, and these were compounded by the various COVID-era restrictions that many of our sites faced.”
Nevertheless, Davies stated in an interview with the AHA that he and his colleagues are “really excited” to be able to share the results from the EMBOLISE study at ISC 2024, once again citing the “highly significant” reduction they observed in the rate of reoperation in patients who underwent MMA embolisation plus surgery.
“We also found that adding this procedure, which of course carries risks with it, did not cause significant safety problems—we did not have any worsening neurologic deficits,” he concluded. “This is a procedure that appears to dramatically reduce [recurrence] and help the patients.”