The MEMBRANE randomised controlled trial (RCT)—presented at the 2024 Society of Vascular and Interventional Neurology (SVIN) annual meeting (20–22 November, San Diego, USA) by Ansaar Rai (West Virginia University Rockefeller Neuroscience Institute, Morgantown, USA)—has produced fresh evidence on the benefits offered by middle meningeal artery (MMA) embolisation as an adjunct to the current standard of care in chronic subdural haematoma (cSDH) patients.
Thanks to these data, MEMBRANE becomes the latest positive MMA embolisation study to have been presented this year, joining the EMBOLISE and STEM RCTs.
“The MEMBRANE randomised clinical trial met its primary effectiveness endpoint, showing a significant, positive treatment effect in favour of Trufill n-BCA [Johnson & Johnson MedTech Neurovascular] for middle meningeal artery embolisation over standard of care,” Rai said. “The odds ratio favoured MMA embolisation in both the surgical and non-surgical cohorts, and the treatment effect was significantly higher in the larger, surgical cohort, with a clear positive trend in the smaller, non-surgical cohort. Based on the functional outcome analysis at three months, Trufill n-BCA was non-inferior to standard of care—and it almost achieved superiority.”
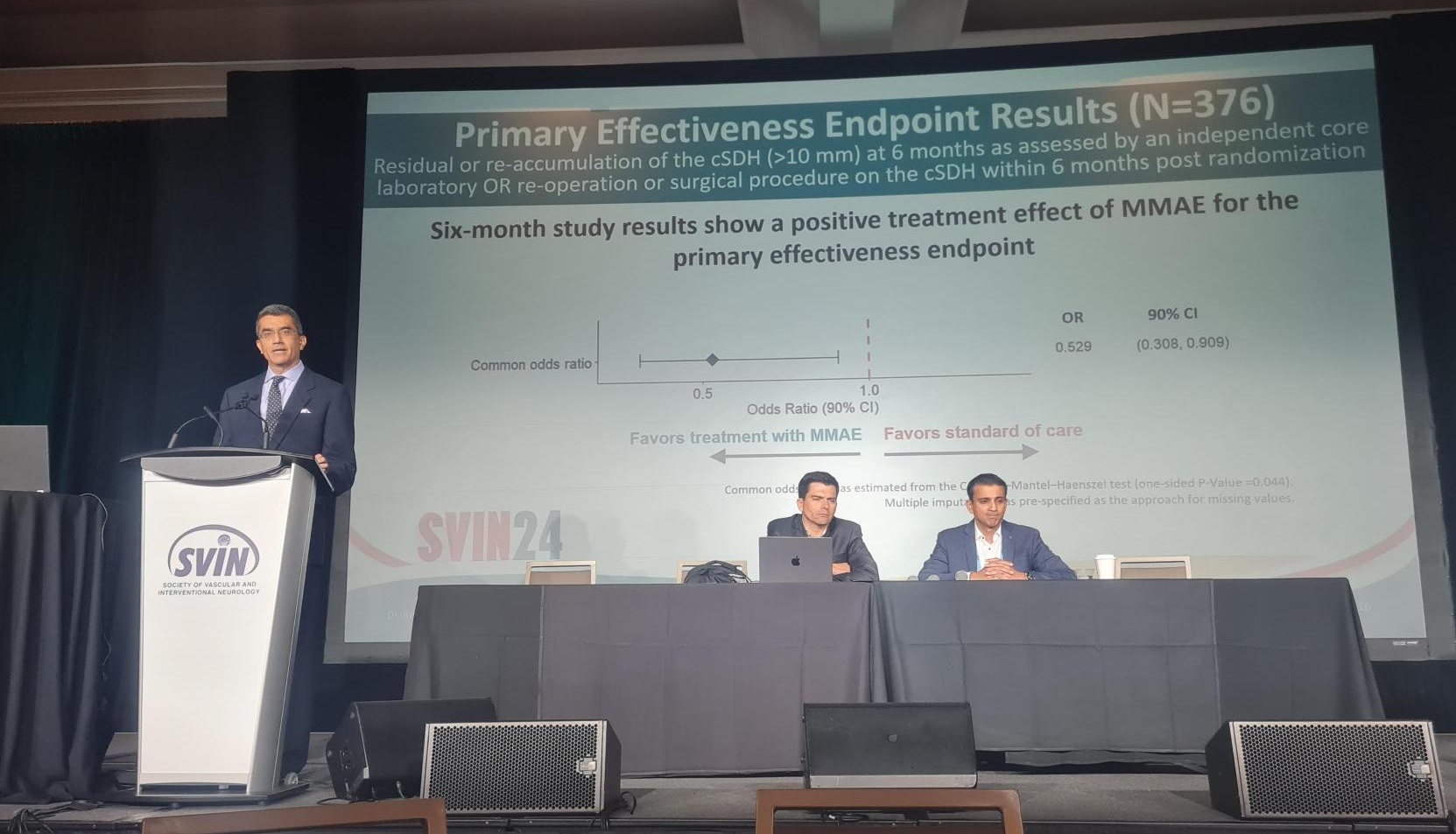
With Rai and Christopher Kellner (Mount Sinai Health System, New York, USA) as co-principal investigators, the prospective, multicentre, open-label MEMBRANE RCT enrolled a population of 376 cSDH patients to evaluate the safety and effectiveness of MMA embolisation with the Trufill n-BCA liquid embolic agent. Its primary effectiveness endpoint was twofold: residual cSDH or re-accumulation (>10mm) at six months, or reoperation or surgical cSDH treatment within six months post-randomisation. The study’s primary safety endpoint was the occurrence of any adverse events through six months, while good functional outcomes at three months, mean change in haematoma volume, development of new seizure onset and modified Rankin scale (mRS) distribution change were among several secondary endpoint measures.
From a total of 376 enrolled patients, 265 were randomised to receive surgical treatment and 111 were assigned to non-surgical medical management. Further randomisation within these groups saw 133 patients allocated to surgery plus MMA embolisation (treatment arm) and 132 allocated to surgery only (control arm), while 55 were assigned to non-surgical management plus MMA embolisation (treatment arm) and 56 were assigned to non-surgical management only (control arm). Some 225 patients in the surgical management group and 78 in the non-surgical medical management group completed the study’s six-month follow-up visit and were therefore able to be included in intention-to-treat analyses. Enrolment in the study took place across 28 US sites as well as two centres in China.
Regarding demographic and baseline characteristics of the study population, Rai noted an average age of roughly 70 years, a predominance of male gender, and headache being the most common presenting symptom. He also highlighted the fact that about one quarter of the patients in MEMBRANE were on antithrombotic medications. In terms of haematoma characteristics, there was an even distribution between left- and right-sided target cSDHs, and a mean haematoma thickness close to 15mm in the surgical cohort versus around 16mm in the non-surgical cohort. Rai further commented that, “as expected”, the average midline shift was “much higher” in the surgical group.
“Procedural information showed that the majority of patients’ procedures—almost 85%—were performed under general anaesthesia,” he added. “Radial access was used in about half of the cases. Target embolisation was achieved in almost 99% [of cases] in the surgical and 100% in the non-surgical cohorts. For surgical procedures prior to randomisation, the most common was burr-hole, followed by craniotomy, followed by SEPS [subdural evacuating port system] and other drains.”
Arriving at MEMBRANE’s primary effectiveness endpoint, the presenter noted a significant and positive treatment effect in favour of MMA embolisation versus standard of care, detailing a common odds ratio (OR) of 0.529 (90% confidence interval, 0.308–0.909) indicating that the failure rate in the embolisation group was almost half of the rate seen in the non-embolisation group. As such, the trial was deemed to have successfully met its six-month follow-up primary endpoint.
In addition, while not individually powered to show treatment benefits, primary effectiveness endpoint results by cohort revealed ORs suggesting favourable outcomes with MMA embolisation versus standard of care in both the surgical management and non-surgical medical management arms of the study. This trend reached statistical significance in the surgical cohort (OR, 0.475) but not the non-surgical cohort (OR, 0.615), Rai reported. As per the primary effectiveness endpoint, failure rates across the study arms were as follows: 8.5% with surgery plus embolisation; 20.2% with surgery only; 20% with non-surgical medical management plus embolisation; and 27% with non-surgical medical management only.
Primary safety endpoint results across 371 eligible patients showed a “fairly similar and even distribution” of all adverse events between the embolisation and non-embolisation groups at six months, according to Rai. There was a 3.3% rate of procedure-related serious adverse events and a 2.2% rate of device-related serious adverse events across 181 patients who received MMA embolisation. In addition, the rate of all strokes—either minor or major—was between 2–3% in both the embolisation and non-embolisation cohorts.
Regarding one of MEMBRANE’s key secondary endpoints, Rai stated that three-month good functional outcomes—meaning an mRS score of 0–2 or a score that did not worsen in patients with a baseline mRS of 3—were observed in 85.3% of patients who received embolisation compared to 77% in patients who received surgical or non-surgical management alone. He went on to relay that, as such, MMA embolisation was deemed statistically non-inferior to the standard of care and—owing to a non-inferiority margin of –0.12 and a risk difference of 0.073—the treatment “almost achieved superiority”.
Further ‘as-treated’ analyses of mRS distribution changes revealed that all-cause mortality was “much lower” in the trial’s embolisation arm (4%) versus the non-embolisation arm (12.4%), and six-month mRS shift analyses—while not statistically powered—found a positive trend favouring MMA embolisation in the surgical arm.
“The primary effectiveness endpoint subgroup analysis by age showed that there was a treatment effect in all age groups, across all [study arms], but the most significant treatment effect was in patients over the age of 75 in the surgical cohort,” Rai commented. “This represents the most vulnerable population, with large haematomas that require surgical evacuation, and adjunctive MMA embolisation was found to have the strongest treatment effect in this age group.”
Touching on three additional secondary effectiveness endpoints from MEMBRANE, the presenter reported a higher rate of complete cSDH resolution with MMA embolisation, compared to both surgical and non-surgical management alone, as evaluated by an independent core laboratory at three and six months. Rai also relayed that rebleeding probability rates—assessed in the same way—were shown via Kaplan-Meier curves to be lower in patients undergoing MMA embolisation, adding that rebleeding was most common in the first three months post-randomisation when it did occur. Finally, he reported a “much lower” rate of surgical reoperation in the trial’s MMA embolisation groups, with reoperations that were required typically taking place within three months as well.
“The question that was asked—similarly to the other trials—was whether MMA embolisation has a role [to play] in the treatment of chronic subdural haematomas,” Rai noted, providing additional context on the study. “The reason this question is important is because we have a growing patient population; the fastest-growing segment of our society is the over 65s. And, the incidence and prevalence of subdural haematomas in this population is increasing. We know it’s one of the most common neurosurgical diagnoses […] and leads to a cascade of disability. The [eventual] eligible population is estimated to be potentially larger than large-vessel strokes.”