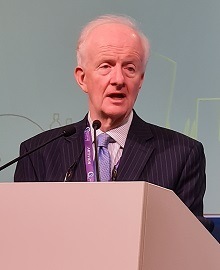
“The time has definitely come to look at the evidence, and redo these studies,” posited Alun Davies (Imperial College London, London, UK), putting forward his argument that the NASCET and ECST clinical trials “need to be reconducted” at this year’s Charing Cross (CX) Symposium (25–27 April, London, UK).
Much of Davies’ argument centred around the fact that best medical therapy—the comparator arm against which carotid endarterectomy (CEA) was assessed, and found to produce clinical benefits in carotid artery stenosis patients, in both of these studies—is “significantly better than it was” at the time.
“We are relying on evidence from 1992, and I would say the playing fields have completely changed,” he noted.
After briefly outlining discrepancies between the North American NASCET and European ECST trials regarding how internal carotid artery stenosis was defined—with ECST having a higher threshold for severity—Davies also reminded the audience that NASCET observed a 3.3% stroke/death rate at one month in its medical therapy arm, compared to roughly 5–6% with CEA.
He then alluded to a 2003 paper by Ross Naylor (University of Leicester, Leicester, UK) et al that, based on primary and secondary analyses of both trials, concluded that not all patients with symptomatic stenosis >70% will benefit from CEA. Davies went on to cite a pooled analysis of prior randomised trials, published in the European Journal of Vascular and Endovascular Surgery in 2021, that found a lower stroke risk with best medical therapy in earlier studies (1981–1996) versus later ones (2000–2008).
Furthermore, he continued, recent research has shown that targeting and lowering a patient’s cholesterol, and initiating best medical therapy more quickly, can reduce adverse event rates by up to 80% early on. Applying this reduction to the rate of 3.3% seen in NASCET, he theorised that stroke/death incidence could now be as low as 0.7% with today’s best medical therapy.
This, coupled with uncertainties surrounding if—and in which cases—CEA is a cost-effective procedure, led Davies to reiterate that more randomised controlled trial data are now needed to re-evaluate the benefits of surgery versus medical therapy.
“We would certainly all prefer to take a tablet than have an operation or have a metal stent stuck in our neck,” Davies asserted. “I would suggest that, unless we get better evidence, […] we will not be doing CEA much in 2025.”
At the close of his presentation, the speaker highlighted the COMeT study—a proposed randomised trial comparing carotid intervention and best medical therapy that he and his colleagues are currently preparing to submit to the UK National Institute for Health Research (NIHR) for the second time, and for which they intend to enrol more than 2,500 patients.
With the COMeT investigators being open to the idea of expanding outside of the UK, Davies urged interested parties to contact him via [email protected], or his colleague Matt Bown (University of Leicester, Leicester, UK) via [email protected].
Moderator Domenico Valenti (King’s College London, London, UK) said he “completely agreed” with Davies’ views, describing NASCET as an “obsolete” trial and stating that newer best medical therapies are “more than effective”.
Valenti also raised the issue of patient compliance when it comes to taking multiple medications over an extended time period—leading Davies to aver that, “if you actually take the time to educate your patients properly, […] and spend 10–15 minutes talking to them as you might do when consenting them for an intervention, you might find that your compliance is better”.
“I fully accept there are patients who may be intolerant of medications, and could benefit from an intervention, but I think the jury needs to have new data to be able to consider,” Davies concluded.