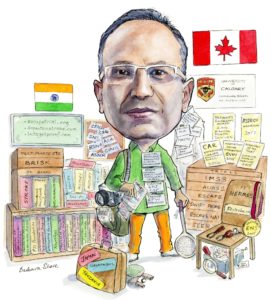
Mayank Goyal is a professor in the Department of Radiology and Clinical Neurosciences at the University of Calgary, Canada. He is the Director of Imaging and Endovascular treatment at the Calgary Stroke Program. Goyal’s passion and main research interest is acute stroke imaging, workflow and intervention. In his spare time he likes travelling, playing racket sports, golfing, and reading.
What drew you to medicine and interventional neuroradiology in particular?
I was a more of a physics, math and logic kind of kid and grew up playing sports. I do not really know how I ended up in medicine. However, once I got into medicine, I was clear I was interested in neuro…. for me it was like the ‘the last frontier’ in the understanding of functioning of the human body.
Who were your mentors and what impact have they had on your career?
I did my medical training and residency at the All India Institute of Medical Sciences in New Delhi, India. During my training there the people who had the greatest impact on my career were Raju Sharma and N K Mishra. During those formative years, they taught me the importance of a patient-centric approach to practice of medicine, the value of old-fashioned hard work and the power of collaboration. Subsequently, I moved to Toronto, where I did a fellowship at the University of Toronto under the supervision of K terBrugge and R Willinsky. Working under these legends of Neurointervention, helped me understand the value of good data, evidence-based medicine and how necessary it is to focus on an issue or problem and stick to it.
You have been practising for a number of years. How have you seen the field of interventional neuroradiology change and develop over that time?
 I remember as a resident spending time tying detachable balloons to microcatheters. Practically there were very few conditions one could treat (brain and spine arteriovenous malformations, carotico-cavernous fistulas) and there was also limited tools. Then the mega-advancement was: coiling of aneurysms. As expected, we were initially treating only those aneurysms that could not be surgically treated e.g. basilar tip aneurysms. The ISAT trial changed all that and led to a major jump in neurointervention volumes. Of course, clearly the biggest advancement by far for the field is the recent change in the treatment of acute ischaemic stroke. I do not think there has been a similar precedence in the whole of medicine where five randomised controlled trials show the same result.
I remember as a resident spending time tying detachable balloons to microcatheters. Practically there were very few conditions one could treat (brain and spine arteriovenous malformations, carotico-cavernous fistulas) and there was also limited tools. Then the mega-advancement was: coiling of aneurysms. As expected, we were initially treating only those aneurysms that could not be surgically treated e.g. basilar tip aneurysms. The ISAT trial changed all that and led to a major jump in neurointervention volumes. Of course, clearly the biggest advancement by far for the field is the recent change in the treatment of acute ischaemic stroke. I do not think there has been a similar precedence in the whole of medicine where five randomised controlled trials show the same result.
In your opinion, what has been the most practice-changing advance in terms of treatment options and devices?
The answer is obvious: endovascular thrombectomy for acute stroke. One has to remember that there are few opportunities in the practice of medicine where one is curative (as opposed to preventive). When we treat an unruptured aneurysm or AVM: we are trying to prevent risk of future rupture. Even when we treat a ruptured aneurysm, there is no immediate impact on the patient. This is totally different in an acute ischaemic stroke due to large vessel occlusion (LVO). It is like magic; pull the clot out and the patient becomes better…. the Lazarus effect!
However, in terms of technology, technique and training, we have scope for improvement. I had proposed the use of TICI 2c many years ago and now it is being used in mainstream. I think we should be looking at both time to and the quality of reperfusion: groin to first past TICI 2c/3, not TICI 2b/3. This will take into account not only the devices and technique but also individual skill in getting to the clot and successfully removing it.
What is on your wish list in terms of the future development of stroke therapy?
The single biggest problem we collectively face right now is getting the correct patient to the correct hospital quickly. We have the obligation to make endovascular thrombectomy (EVT) available to everyone as early as possible after stroke onset. Besides the need for better tools in the field to detect patients likely to have an LVO, we also need sensible, practical policy and organisation to have an appropriate distribution of EVT capable stroke centres and corresponding triage capabilites.
You are the principle investigator of the ESCAPE and SWIFT-PRIME trials, which looked at the use of stent retrievers and showed that their use improved outcomes. What was the impact of these studies, and what further advancements do you see on the horizon?
These two studies were among the five that made EVT the standard of care. As I have mentioned before, this is a revolution in stroke care with worldwide impact and gives significant hope for an otherwise dismal disease. As we analyse data from these studies and from the HERMES collaboration, it is becoming hard to find a sub-group in which EVT does not work. We have been able to show benefit in patients at any age, either sex, irrespective of time of onset, severity of stroke, site of occlusion. There is benefit in patients with moderate to good ASPECTS and/or collaterals. And we have been able to confirm the importance of time and speed. Onset to imaging decides the likelihood of favourable imaging and in those with favourable imaging, imaging to reperfusion decides the likelihood of favourable outcome.
Patient selection had a big role to play in the success of those trials. How was the protocol defined and do you believe that this should be used to select all thrombectomy-eligible patients going forward? Are other selection criteria/modes still viable?
Most of recent trials were designed to choose patients that had the highest likelihood of showing effect of treatment. This made sense at the time given the ‘failure’ of previous trials to show benefit of EVT. Even the trials that did not have very conservative inclusion criteria (like MR CLEAN) was also ultimately enrolling patients with good ASPECTS. The final result was an overwhelming effect size (including in the recent late window trials). Clearly there are patients who were not enrolled in the trials that were at the margins of the inclusion criteria that will also benefit from treatment. We have to keep that in mind as we move forward. Also, one thing that cannot be argued against is: time is brain. Thus, imaging protocols and patient selection should be simple, widely implementable and not ime consuming. Given ease of access of CT and no contraindications, in most situations CT should be the preferred modality and the protocol should include a CT head (to exclude haemorrhage) and a CT angiogram (to detect LVO; there is the collateral benefit of providing the vascular anatomy to plan the EVT). In addition, one has to think of the fastest and most robust way to exclude patients who have a large core. This is why we have made a modification to our CTA protocol to multiphase CTA that allows evaluation of collaterals, making it easier to detect LVO and helping to confirm the ASPECTS reading. I believe that this CT, mCTA protocol is sufficient, efficient and widely implementable.
What are your other current research interests?
We are currently running a worldwide trial called ESCAPE NA1 trial testing the added benefit of neuroprotection (we are testing the compound NA1) in patients undergoing EVT. At the moment we have 282 patients enrolled. I have just finished the UNMASK EVT study aimed at trying to understand the variance of physician decision making in acute stroke. It is the first study of its kind and is based on the principles set forth by Nobel Laureate Dan Kahneman.Additionally, I continue to push for evidence based, data-driven practice of medicine and we are planning additional RCTs and registries. I am building a web-based platform for increasing the efficiency of stroke research through crowd-review and crowdfunding. The site is called letsgetproof.com.
What was your most memorable case and what did you learn from it?
I remember clearly the first stroke case I treated using Solitaire in 2009. At that time it was not close to being approved and we had just got it on the shelf for stent-assisted coiling. This young 45 year old woman had come in with dense left hemiplegia. She was an immigrant who was doing three jobs to make ends meet. She had an ICA-M1 occlusion. I finished the entire case, skin to skin in under 15 minutes using the stent retriever. At that time it felt like magic. She fully recovered on the table and said: Can I go back to work? The case was memorable for many different reasons: the ‘magic’ of opening the vessel, the tenacity of the human spirit and of course, the procedural efficiency with better technology
What are your interests and hobbies outside of medicine?
I love to travel with my family, see new cultures and places and meet new people. As a family we also love racket sports, and board games. I play golf once in a while with my sons (although I never keep score). I love to read all kinds of books including mystery, science fiction, history, non-fiction and philosophy. Some of the books I have recently read and liked are by Michener, Asimov, Gawande, Malcolm Gladwell and Taleb. I also love to write; I write opinion pieces and editorials in flights. I do love recent TV shows: Breaking Bad, Homeland etc. My wife and I love to socialise; we have a big friend circle and have a rule about always having Saturday dinner with friends
Fact File
Academic appointments
- Professor of Radiology and Clinical Neurosciences, University of Calgary, Diagnostic and Interventional Neuroradiology
- Director, Imaging and Endovascular treatment, Calgary Stroke Program
Awards (recent)
- 2018 CAR–Distinguished Career Achievement Award
- 2017 ASTECH (Alberta Science and Technology) Innovation Award
- 2016 President’s Excellence Award: Research. Alberta Health Services
- 2015 Researcher of the year: Clinical faculty. Cumming School of Medicine
- 2015 Contributions to Innovation in the field of Neurointervention. Society of Vascular and Intervention Neurology
Research
- ESCAPE Worldwide randomised controlled trial carried out at 22 sites.
- SWIFT PRIME 39 sites across North America and Europe.
- SEER Patient level meta-analysis of trials that used the Solitaire device.
- HERMES Collaboration of seven randomised controlled trials testing endovascular thrombectomy. One of the unique aspects of the collaboration is that we re-evaluated all the images centrally. It is the largest patient level database of its kind and it has allowed us to evaluate many of the sub-groups.
- ESCAPE NA1 Ongoing worldwide trial tested the added benefit of neuroprotection in patients undergoing endovascular thrombectomy
- UNMASK EVT First study of its kind assessing factors contributing to physician decision making in taking patients for endovascular thrombectomy based on the principles of neuroeconomics
Experience
- 2000–06 Associate Professor Department of Radiology Ottawa Hospital, Ottawa
- 2000 Clinical Fellow, Neuroradiology Ottawa Hospital-Civic Campus, Ottawa, Canada
- 1998 –2000 Clinical Fellow, University of Toronto, Toronto, Canada
- 1996–98 Assistant Professor, Neuroradiology, All India Institute of Medical Sciences, New Delhi, India









