The year 2017 marks the 50th anniversary for spinal cord stimulation therapy which was first used to treat pain in 1967. To celebrate the occasion, NeuroNews spoke to a number of pioneers in the field about how they have seen spinal cord stimulation therapy change and develop over the years and where they hope to see it improve and grow in the future.
In your opinion, what has been the most important development in spinal cord stimulation?
Giancarlo Barolat: The first 35 years of spinal cord stimulation development were dedicated mostly to figure out where to place the electrodes to activate the correct pain-reducing pathways. The last five to six years have been dedicated to try to understand the language (or languages) of the nervous system and how to communicate with it in a more meaningful way. This has meant more efforts placed on evaluating different electrical parameters and waveforms. These additional efforts have brought a new dimension in the efficacy of spinal cord stimulation.
Christophe Perruchoud: Neuromodulation grows exponentially and major developments are numerous. Since the first description of spinal cord stimulation, understanding of underlying mechanisms of action, although still incomplete, made significant progresses. High-quality studies showed strong evidence about the efficacy and cost effectiveness of the therapy in several chronic pain conditions and undoubtedly contributed to the development of spinal cord stimulation. Over the past years, the reliability of implanted devices has considerably improved. Rechargeable batteries and MRI compatibility systems are also a remarkable step forward. Finally, paraesthesia-free stimulations, such as high frequency or burst stimulation, deeply transformed the field of neuromodulation.
Simon Thomson: If I have to think about what is THE most important development in spinal cord stimulation, it has to be that through the accumulation of high-quality clinical studies, the clinical and cost effectiveness in well-selected patients is proven. As such, it is reimbursed by both public and private healthcare systems in the UK. This means that patients who need and will benefit from this treatment are and will receive it. It is a matter of healthcare politics to make it happen in every health economy.
Everything else that is surgically and technologically available today is about improving the clinical and cost effectiveness making it more affordable for more patients.
What have been the major challenges associated with spinal cord stimulation over the last 50 years?

Giancarlo Barolat: The first two decades were marred with a variety of technical problems affecting the implanted devices. The most vexing one was the frequent breakage of the implanted electrodes, which required numerous surgical revisions. Issues with the pulse generators and their circuitry were also not uncommon. The quality and reliability of the devices has made quantum leaps in the past decade and technical issues are now much less of a problem. The exact location of the targets in the nervous system has also been a tremendous challenge. As of today, in many instances we are still not sure where the leads should be placed or where the most effective target areas are.
Christophe Perruchoud: One of the major challenges is the difficulty in establishing spinal cord stimulation as a stand-alone treatment, as well as surgery or drugs, and not only as a last chance therapy. The high costs and only partially understood mechanisms of actions probably acted as obstacles to a better acceptance of therapy.
Simon Thomson: Changing the perception of spinal cord stimulation from an interesting curiosity for a minority of patients to a clinical service that can treat a population of patients.
Where are the key opportunities for growth within the area of spinal cord stimulation and how do you see devices and therapy developing and changing in the future?
Giancarlo Barolat: There is a tremendous growth opportunity in this field. Stimulating the nervous system can affect many different conditions, including pain, bladder/bowel dysfunction, epilepsy, depression, obesity, high blood pressure, angina pain, headaches and even conditions like rheumatoid arthritis. Future research will be concentrated on different target areas in the nervous system as well studying how various electrical parameters may affect different body functions and dysfunctions. Micro technologies with miniaturisation of the devices, improved battery life, a variety of waveform will unleash our ability to interface in a more effective way with the nervous system and body dysfunction.
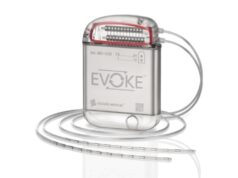
Christophe Perruchoud: Each manufacturer developed its own mode of stimulation. For obvious economic reasons, it is impossible to provide each patient with the full spectrum of stimulations’ modes. All-in-one devices would unquestionably be an asset. Closed-loop technologies may also strongly contribute to a therapy more tailored to a patient’s individual needs.
Neuromodulation techniques and spinal cord stimulation in particular are symptomatic and palliative therapies. Techniques inducing structural changes or treating the cause rather than the symptoms could revolutionise the place of neuromodulation procedures in the algorithm of treatment. Stimulation of the medial branch nerves to treat back pain of muscular origin is a good example of it. Built-in tools such as gyroscope and accelerometer would also allow us to obtain objective outcomes and help to overcome the subjectivity in measuring pain. Moreover, all the implanted devices are sensitive to cyber hacking, which calls for a constant security tightening and firmware upgrading.
Simon Thomson: Technological improvements in spinal cord stimulation have meant that the sometimes dominant back pain component of chronic neuropathic back and leg pain (also known as Failed Back Surgery Syndrome) can be treated as well as the leg pain component. This has brought many more patients to the treatment. There are still 10 to 20 fold more patients with this condition who could be treated than we currently are referred.
Outside of pain, what do think are or could be the most useful applications for spinal cord stimulation?
Christophe Perruchoud: Modulation of the sympathetic component by spinal cord stimulation could be applied in the future to treat bronchospasms associated with asthma, constipation and other gastrointestinal motility disorders and possibly metabolic disorders such as diabetes.

Simon Thomson: There are many pain indications that have not received adequate clinical research such as ischaemic pain (chronic critical limb ischaemia and refractory angina) as well as visceral pain (such as chronic pancreatitis).
Spinal cord stimulation is used to augment neurological recovery after spinal cord injury in spinal injury research centres. Spinal cord stimulation has been used in research studies for heart failure, heart rhythm stabilisation and augmentation of chemotherapy for brain tumours.
Neurostimulation generally is used as a therapy in all organs of the body in a broad array of chronic illnesses. Interfacing advanced sensing and stimulating devices with natural systems of the body is the direction of development for this field.
Giancarlo Barolat is director of Barolat Neuroscience, Denver, USA and Past President of the International Neuromodulation Society
Christophe Perruchoud is at the Department of Anesthesiology and Pain Management, Center for Neuromodulation, Hospital of Morges, Switzerland
Simon Thomson is consultant in Pain Medicine and Neuromodulation at Basildon and Thurrock University Hospitals NHS Foundations Trust, Basildon, UK, and Past President of the International Neuromodulation Society