While the randomised controlled SELECT2 trial initially found that patients with large-core ischaemic stroke receive a greater benefit from thrombectomy compared to medical management, a secondary analysis of data from the study has now shown that the benefits of thrombectomy are less certain in patients with severe hypodensity of ≥26ml within their ischaemic lesions—and the likelihood of a hemicraniectomy being required is increased in these patients as well.
This secondary analysis of SELECT2—which was presented earlier today at the European Stroke Organisation Conference (ESOC; 15–17 May, Basel, Switzerland) by Vignan Yogendrakumar (Royal Melbourne Hospital, Melbourne, Australia), one of the lead authors of the study—used imaging and outcome data from the 322 large-core ischaemic stroke patients included in the trial.
Researchers hypothesised that the occurrence of severe hypodensity, which is indicative of more evolved tissue injury, may modify the effect of thrombectomy. For the study, they defined severe hypodensity as an attenuation in the ischaemic lesion of less than 26 Hounsfield units, while a modified Rankin scale (mRS) score of 0–3 constituted a favourable outcome.
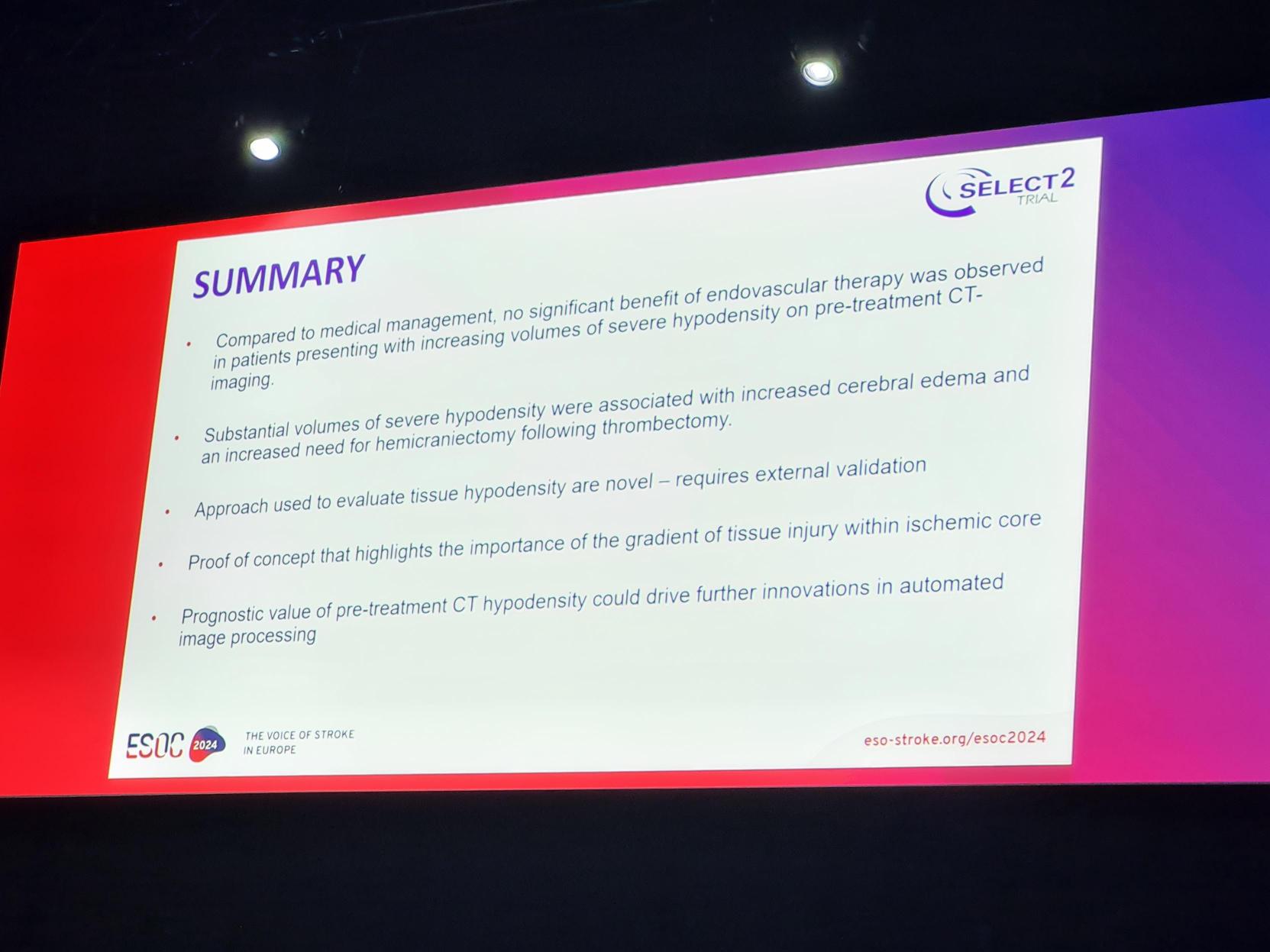
The results showed that, with increasing volume of severe hypodensity, the odds of a favourable outcome decreased. Investigators found that, at a cut-off of ≥26ml of severe hypodensity, thrombectomy was no longer associated with a favourable outcome compared to medical management. In addition, the odds of requiring a decompressive neurosurgical procedure known as a hemicraniectomy were increased.
“This study provides evidence supporting the concept that the gradient of tissue injury can influence clinical outcomes and the treatment effect of endovascular therapy,” said Yogendrakumar. “It is, however, important that these findings be validated with independent data, as the techniques used in this analysis are relatively novel. If validated, the prognostic value of assessing CT [computed tomography] hypodensity could be used to assist with bedside decision-making, accelerate innovations in automated imaging processing, and could even be used as a biomarker for trial recruitment of new therapies designed to limit reperfusion injury.”