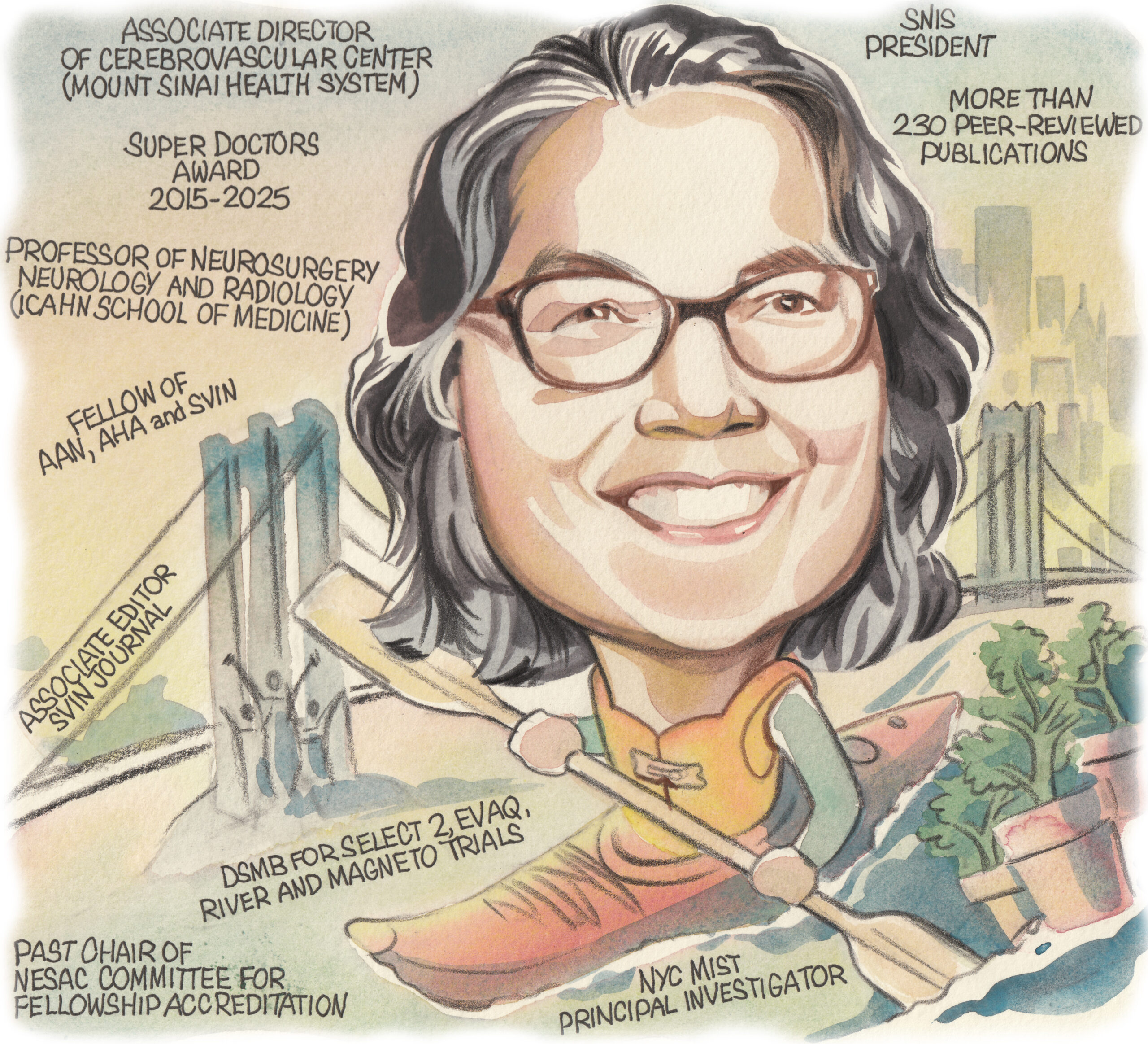
Following in the footsteps of many of her neurointerventional mentors as president of the Society of NeuroInterventional Surgery (SNIS), Johanna Fifi (New York, USA) has proudly led the society’s mission to expand and enhance the cerebrovascular field throughout the past year. In her current roles as associate director of the Cerebrovascular Center and director of the Pediatric Cerebrovascular Disorders Program at Mount Sinai Health System, she devotes her time and expertise to furthering treatments for adults and children alike with neurovascular diseases. Here, Fifi—a professor of neurosurgery, neurology and radiology—discusses her career to date in addition to key areas of promise in the neurointerventional field.
What initially attracted you to medicine, and the cerebrovascular field specifically?
What initially drew me to medicine was a love of the sciences and a deep sense of responsibility and empathy—I wanted to be the kind of person others could trust in their most vulnerable moments. Medicine offered a career where I could not only help people physically but see them fully, and help allay their fears, give them appropriate hope, and support their dignity.
The cerebrovascular field specifically appealed to me because of that combination of humanity, precision, and also urgency. With stroke and everything else that we treat, you’re not just treating a condition but often treating to preserve someone’s ability to speak, to move, to think—all that makes them who they are. When I was introduced to the concept of neurointervention, I could not believe how much of a meaningful combination of knowledge, your hands, engineering and creativity it was to do this work.
Which clinicians and researchers have been your most valued mentors, and in what ways have they impacted your career?
There are many, and I feel incredibly lucky for that. I have had mentors at many stages and in several domains, including clinical, leadership and scientific. For clinical care, I have had mentors throughout my career that have influenced me. Stroke neurologists Rodney Bell, Steven Warach and Chelsea Kidwell have taught me how to be an empathetic clinician and to treat based on the science. In my neurointerventional training, I am grateful to William O Bank for showing me the ropes in the transition to a proceduralist and for many other life lessons. This continued with Philip M Meyers, John Pile-Spellman and Sean Lavine. Alejandro Berenstein has been my most longstanding professional mentor, friend and partner. I consider him as family. Finally, J Mocco has been in inspiration as a partner, and has really been a shining example of how to lead from the heart.
What are your main reflections from your tenure as SNIS president?
My tenure as SNIS president has been one of the most rewarding and enlightening chapters of my career. It has been truly remarkable to follow in the footsteps of prior leaders of our field, dedicated to the mission of improving the lives of our patients afflicted with cerebrovascular disease, working with our dedicated board and members as well as other global societies around the world to enhance science, education and knowledge through networking, and access to care for our patients. The SNIS staff, board and membership stand out as truly remarkable for their dedication to our mission.
How would you say the SNIS has evolved in the years since you first joined the society?
I became a senior member of the society in 2010, but I attended my first SNIS meeting back in 2004. Since then, I think that the SNIS has evolved into a multidisciplinary society where neurointerventionists from all of our specialties can find a welcome home. Neurologists, radiologists and neurosurgeons alike are welcome. And I think the perspective of each are truly welcome as an additive value to our society. This is unique, and it’s what strengthens and positions our society to lead this field.

Of all the clinical studies and registries you are currently involved with, which do you feel has the potential to make the greatest impact within the neurointerventional space?
This is difficult to answer. There have been so many stroke trials I’ve been involved with in the past that have changed our field. Currently, I’m excited about technologies that are expanding the orbit of our field. Firstly, Stentrode (Synchron)—this has the potential to bring neuroendovascular into the electrophysiology of our brain. Going back to what I said in the beginning, this ability to intermingle with the essence of our humanity, to restore our most human functions, is groundbreaking. Less philosophical but no less impactful, I think the current STRIDE registry (Cerevasc) that we are performing to look at cerebrospinal fluid (CSF) diversion has the potential to impact numerous lives across the world.
What do you feel have been the three most important developments in the cerebrovascular field during your career?
Well, the most impactful without a doubt, in terms of lives touched, has been the evolution of endovascular treatment for stroke. The validation of stroke thrombectomy as a proven and highly efficacious treatment for large vessel occlusion has revolutionised—for many—the landscape of our practice. I am so grateful to have been involved in many of the trials over the last 20 years or so that have shaped this space, including MR RESCUE as a fellow, as well as SWIFT, THERAPY, COMPASS, DEFUSE 3, SELECT2 and DISTALS, to name a few. The coming together of physicians and scientific minds drawn by the possibilities of saving patients’ lives and humanity to prove this therapy is really not surpassed by anything I’ve witnessed in medicine.
I have to mention a disease I hold near to my heart: paediatric arteriovenous shunts. Working with children has been a passion of mine from fellowship, and it has led me to pursue working with Alejandro Berenstein, which I have done for the past 17 years. Progress in the technological achievements we can perform to save these young children’s lives has been revolutionary. I believe that we currently stand at a precipice in terms of understanding the molecular and genetic underpinnings of the disease, and of technological ability, and I am looking forward to unravelling how we can make sure these patients live long and productive lives.
How would you assess the role for thrombectomy in more distal-occlusion strokes following the recently presented trial data in this area?
The role of thrombectomy in more distal-occlusion stroke beyond M2, A1 or P1 locations has been a special interest of mine as well. I am serving a role on the nationwide National Institutes of Health (NIH)-funded STEP platform trial on distal occlusions to clarify the benefit of thrombectomy in these more distal occlusions—often termed medium-vessel occlusions (MeVOs). While recent studies like DISTAL and ESCAPE-MeVO have planted doubts about the treatment, I believe that patient selection is crucial. We will need the upcoming data to elucidate the parameters of benefit.
Besides your own work, what is the most interesting piece of neurointerventional research you have seen over the course of the past year?
I think that the conglomerate evidence that has amassed for middle meningeal artery (MMA) embolisation for subdural haematoma over the past couple of years via multiple randomised trials (MEMBRANE, STEM, EMBOLISE and MAGIC-MT) has created a real shift in treatment paradigms. This is interesting to me based on the sheer number of patients affected and helped.
What advice would you give to people embarking on a career in the cerebrovascular field?
The sky is the limit. Think creatively but respect the knowledge gained from the past. This is a field that is maturing—learn from your mentors but keep an open mind for the future.
Last but not least, what are your hobbies and interests outside the field of medicine?
Despite or perhaps because of a demanding work schedule, my interests outside of work are varied. They largely lie with my immediate family—my wife, and two kids aged 12 and 8. Though it may not seem intuitive, living in New York City, we enjoy spending time outdoors together. I love getting out cycling or on the water kayaking, or going upstate in the mountains, hiking and visiting farms on weekends. Recently, I’ve taken the outdoors inside by setting up a little indoor garden with flowers and herbs that we can use for cooking, which I enjoy. Living in the city also gives me the opportunity to indulge—usually with friends—in musicals and plays, including seeing my daughter in a production of Frozen Junior earlier this year! Lastly, I really enjoy travelling, which we do often to visit extended family, but I also get to travel a bit for work. I love exploring new places and learning about history and culture.
FACT FILE
Current appointments:
- 2023–present: Professor of Neurosurgery, Neurology and Radiology, Mount Sinai (New York)
- 2021–present: Director, Pediatric Cerebrovascular Disorders Program, Mount Sinai
- 2018–present: Associate director, Cerebrovascular Center, Mount Sinai
Education:
- 2007–2008: Senior fellow in Neurointerventional Radiology, Columbia University (New York)
- 2006–2007: Junior fellow in Neurointerventional Radiology, Washington Hospital Center (Washington DC)
- 2004–2006: Fellow in Vascular Neurology and Stroke MRI, National Institutes of Health (Bethesda)
- 2001–2004: Resident in Neurology, Thomas Jefferson University Hospital (Philadelphia)
- 1996–2000: Doctor of Medicine, Boston University School of Medicine (Boston)
Honours (selected):
- 2015–2025: Super Doctors award
- 2015–2025: Top Doctors award
- 2010: Young Hearts Award for Achievement in Neurovascular Science and Medicine (AHA/ASA)









