This advertorial, sponsored by Medtronic, is intended for readers outside of the USA.
Mechanical thrombectomy may be the standard of care for acute ischaemic strokes caused by a large vessel occlusion (LVO), but even this established and trusted procedure fails to achieve adequate recanalisation in close to one third of cases, and at an even lower rate after the first pass. However, the practice of deploying two stentrievers simultaneously as a first-line intervention for clots that are refractory to treatment with a single device has shown promise and is now gaining traction—with Pedro Vega (Hospital Universitario Central de Asturias, Oviedo, Spain) and colleagues recently publishing initial experiences of this approach in Clinical Neuroradiology. Here, Vega discusses his team’s findings, and usage of the Solitaire X stentriever and Phenom 21 microcatheter (both Medtronic) as part of this novel technique.
Detailing this ‘double stentriever’ thrombectomy technique, Vega says: “An 8Fr balloon catheter is positioned in the ICA [internal carotid artery], and a 0.014-inch guidewire is advanced through a 0.021-inch microcatheter to the target vessel. After passage through the clot, intra-arterial contrast medium is injected to verify the position of the microcatheter distal to the clot. Then, a second microcatheter is placed distally in the same artery or in another branch of the main artery. The stentrievers are deployed by withdrawing the microcatheters in a parallel or Y configuration, and contrast material is injected to evaluate flow after placement of the devices. The proximal balloon guiding catheter is inflated one or two minutes later to arrest blood flow, and the opened stentrievers are removed simultaneously with aspiration using a 60ml syringe.”
According to Vega, the approach is particularly effective as a first choice of treatment in proximal occlusions, especially when the thrombus is located in arterial bifurcations. “This technique is especially useful in these clots, because they have a tendency to jump from one branch to another when thrombectomy is performed with a single device,” he notes. “The increased radial force from a second stentriever might also be especially beneficial in hard, fibrin-rich thrombi that are difficult to penetrate with a single device.”
Initial experiences
‘Rescue therapy’ using two stentriever devices has been reported previously, demonstrating good results. As such, Vega and his colleagues undertook a single-centre, prospective study to assess whether the potential benefits of a two-device approach translate when it is used as a first-line treatment for acute occlusions of the M1 segment of the middle cerebral artery (MCA) and/or terminal internal carotid artery (TICA). Between May and October of 2020, 39 patients (median age=79 years, 58.9% female) were analysed. Study outcomes included successful recanalisation, first-pass effect, procedure times, number of device passes, symptomatic intracerebral haemorrhage, National Institutes of Health Stroke Scale (NIHSS) score at discharge, and 90-day functional independence and mortality.
The study produced largely positive results, with all 39 patients experiencing successful recanalisation—a final modified thrombolysis in cerebral infarction (mTICI) score of 2b/3—and 27 patients (69%) had an mTICI score of 2c/3 after the first pass. Discussing the latter of these findings, Vega says: “Advantages of using a second device include better integration of the thrombus, thanks to increased radial force from the second stentriever, and more complete coverage of it. Integration of the clot increases the retrieval force transmitted to the thrombus and improves the likelihood of successful thrombectomy.”
In the study, Vega and his colleagues also observed three cases of symptomatic intracerebral haemorrhage (7.9%), and no vasospasms. At 90 days, 16 patients (41%) were functionally independent, registering a modified Rankin Scale (mRS) score of 0–2, and nine (23%) had died. In addition, 15 of 27 patients (55.5%) in the first-pass TICI 2b/3 subgroup had a good clinical outcome (0–2 mRS) at 90 days. As such, Vega and colleagues conclude their Clinical Neuroradiology report by stating that their findings suggest first-line double stentriever thrombectomy is safe and effective for M1/TICA occlusions.
Chosen devices
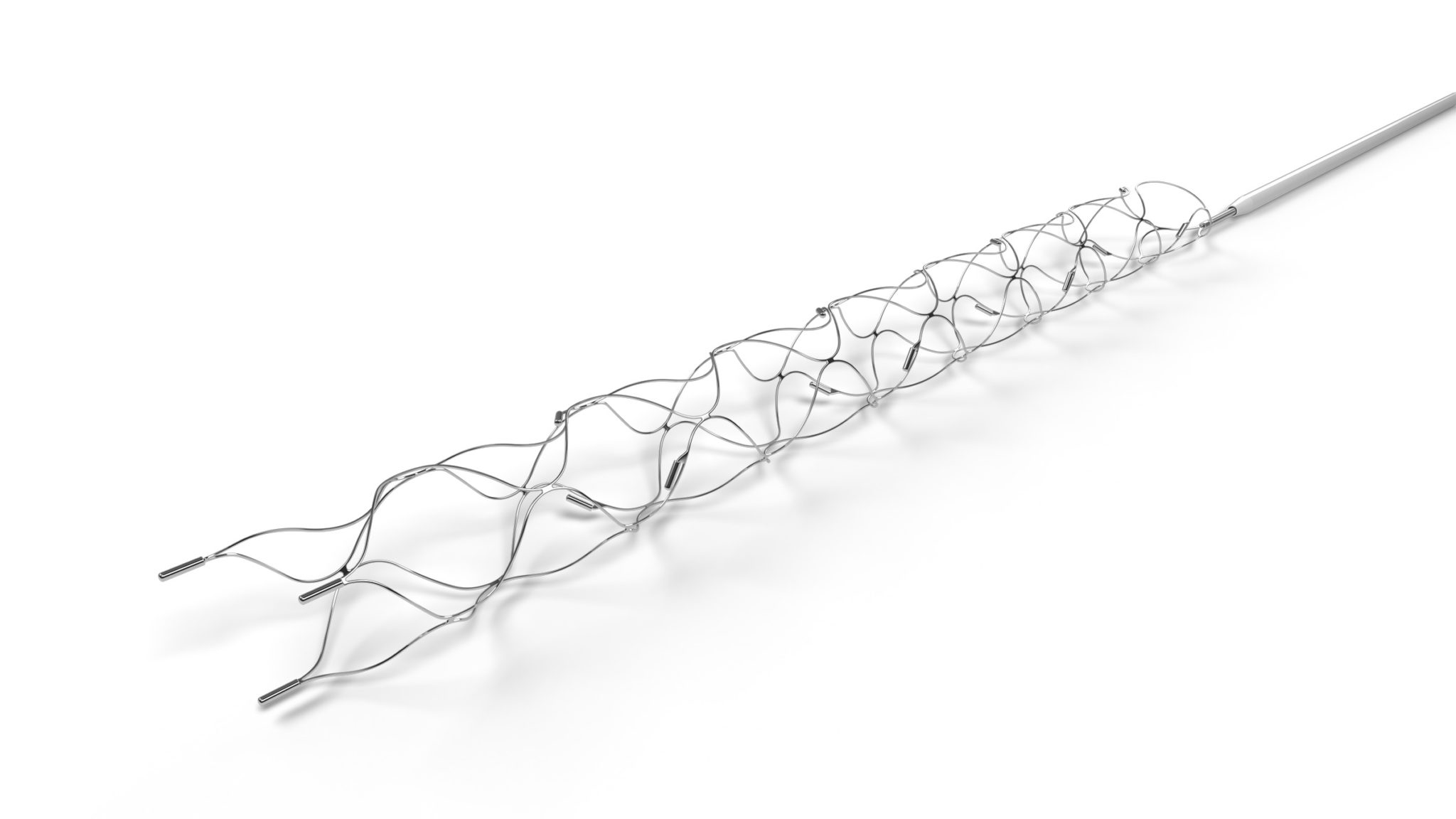
Vega tells NeuroNews that the Solitaire X—which features a unique, parametric design intended to enable dynamic clot integration—was among the most commonly used stentrievers in the study, with 4×40mm and 6×40mm variations of the device being utilised in a total of 19 patients. “While it is hard to say for certain, it makes sense to think that Solitaire’s overlapping structure allows for better interlocking of the two devices, increasing the effectiveness of the technique,” he says. “I would definitely recommend using it as part of the double stentriever procedure. The Solitaire has proven over the years to be a dramatically effective extractor device, whether used on its own or with another device.” And, when asked about the extra cost of deploying two devices instead of just one, Vega notes that an effective technique like this holds the potential to improve first-pass recanalisation rates—avoiding the need for expensive rescue therapies and increasing the percentage of functionally independent patients at 90 days, thus reducing costs in the medium- and long-term. “A cost-effectiveness study would have to be carried out to demonstrate this,” he adds.
Moving on to discuss the fact that one specific microcatheter product, the 160cm version of the Phenom 21, was used in every procedure during this study, Vega highlights the various benefits the device holds. “Phenom 21 is our microcatheter of choice for mechanical thrombectomy in proximal vascular occlusions due to its good navigability and trackability, among other advantages,” he states. “Working with a good microcatheter guarantees the success of the intervention.” Similarly, Vega notes that the use of a balloon guide catheter is his centre’s access system of choice in any thrombectomy procedure, adding: “It is the technique that demonstrates the greatest capacity to block and reverse flow, which has been shown to reduce thromboembolic complications and increase the success of thrombus extraction. It is a key point for the success of the double stentriever technique.”
Future directions
“The most notable benefit is that the percentage of patients in whom a TICI 2c/3 is obtained after the first pass is significantly increased,” Vega claims, homing in on the crux of why he uses the double stentriever approach in M1/TICA occlusions. “I would say that it is undoubtedly a very effective rescue technique when we are unable to extract the thrombus after the first or second pass. Our preliminary results in this series of patients suggest that it is an effective and safe technique if used as a first intention in occlusions located in the TICA and in the M1 segment as well. I would probably recommend that other physicians start using the technique in rescue cases to become familiar with it in order to gradually expand use indications. The next step would be to use it in occlusions located in arterial bifurcations (TICA, MCA and BA [basilar artery]) and in long thrombi located in the M1 segment. However, the generalisation of the use of the technique as a first intention in all cases should be done with caution until more results are available.”
Delving further into the generalisability of the study at hand, Vega concedes several limitations, including its relatively small size, and lack of patient randomisation or a control group. He notes that additional data are necessary before double stentriever thrombectomy can be included in international guidelines as a first-line option for proximal occlusion, and randomised controlled trials comparing the use of single versus double stentriever thrombectomy will further clarify the effectiveness, safety and cost of the latter. Vega also believes that it is essential to carefully assess the possible risks and benefits of this approach before attempting it in individual patients. “In any case, the results are very promising and we are working on the development of an international, multicentric study to demonstrate that our results hold up,” he concludes. “I am sure that, in the near future, we will demonstrate with the highest level of scientific evidence that it is the most effective technique.”
Pedro Vega is the head of Interventional Neuroradiology in the Department of Radiology at Hospital Universitario Central de Asturias in Oviedo, Spain.
DISCLAIMER: The data and content included in this presentation express only the clinical perspective of the presenter. They are completely independent and do not necessarily reflect the opinions of Medtronic.













