Preliminary data on a transvascular platform for subdural haematoma (SDH) treatment—which involves performing middle meningeal artery (MMA) embolisation and haematoma drainage within a single endovascular procedure—were presented at this year’s LINNC Paris course (2–4 June, Paris, France), indicating the safety and feasibility of the approach across a small cohort of patients.
Pedro Lylyk (Clinica la Sagrada Familia, Buenos Aires, Argentina) delivered these initial data, reporting 100% rates of technical and clinical success within 13 non-acute SDH patients.
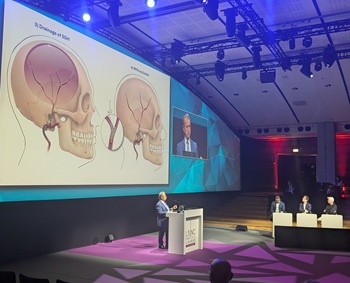
The presenter began by guiding the LINNC audience through the multi-stage procedure, which consists of embolisation of the distal MMA followed by transvascular access to the subdural space, drainage of the haematoma itself through a microcatheter and, finally, proximal MMA occlusion. He also briefly highlighted the potential benefits of combining MMA embolisation with SDH drainage, including lower rates of complications and recurrences, fewer hospital admissions, and a shorter average length of stay, as compared to the standard of care involving two separate procedures.
During his talk, Lylyk asserted that the safety of this novel procedure is predicated on its design, as transvascular access is performed in a ‘safe landing zone’ that can be visualised via conventional imaging tools, thus ensuring no inadvertent damage to bridging veins or other surrounding vascular structures will occur. Another key point he highlighted was the fact that access takes place in a ‘blood-free’ segment of the MMA, alleviating any concerns regarding bleeding upon creation of the transvascular passage to the subdural space.
With Lylyk as principal investigator, EMBODRAIN—a prospective, single-arm study intended to assess the safety and feasibility of this approach—enrolled patients with non-acute SDHs requiring treatment. In the study, 13 out of 15 enrolled patients ultimately underwent transvascular SDH evacuation utilising the Volta neurovascular guidewire (Endovascular Horizons)—a device that delivers radiofrequency energy in order to achieve MMA embolisation.
Here, Lylyk briefly outlined the details of the first-ever patient treated with this technique in Argentina: a 73-year-old man whose SDH had both chronic and acute components, and who presented with right hemiparesis and aphasia. The presenter relayed that he was able to drain more than 80% of the volume of the patient’s haematoma, and the patient was out of bed and walking independently—with significantly reduced paresis—on the second day following the procedure. Follow-up imaging at both three and six months revealed no SDH recurrence, Lylyk added.
Clinical follow-up data across the full EMBODRAIN cohort revealed that every patient achieved at least a return to their baseline modified Rankin scale (mRS) score by the three-month timepoint, with similarly positive results being observed regarding Markwalder grading scale (MGS) scores and motor-strength outcomes. In addition, the study’s radiological follow-up demonstrated significant reductions in SDH thickness, volume and midline shift across all 13 patients, representing a 100% rate of technical success, with no instances of conversion to open surgical drainage being required in six months of follow-up. Zero serious adverse events were seen throughout the study population. Lylyk went on to relay that, overall, no SDH recurrence or progression requiring surgery—nor hospital readmission or deterioration in neurological function—occurred within the study.
“So far, I think the protocol has shown that it is possible to drain the subdural with a microcatheter, in a single procedure, with a high safety profile,” Lylyk posited. “So, think about it; maybe some change in our practice is important.”
“Each time I see this technology, it’s completely amazing to me—especially when you see the drainage through the microcatheter. It’s absolutely incredible,” commented LINNC course director Laurent Spelle (Bicêtre Hospital, Le Kremlin-Bicêtre, France) following Lylyk’s presentation.
LINNC course director Vitor Mendes Pereira (St Michael’s Hospital, Toronto, Canada) added that the procedure is “a crazy idea, but a great idea”, and one that has a chance to make a “real change” in the neurointerventional space, while Italo Linfante (Miami Neuroscience Institute, Miami, USA) commended it as “fantastic, groundbreaking work”. Subsequently, Alejandro Berenstein (Mount Sinai Health System, New York City, USA) noted that “it’s amazing how we are expanding the field”, and Ajay Wakhloo (Tufts University School of Medicine, Boston, USA) pointed out that such transvascular techniques could be used to implant for neuromodulation, biopsies and many more frontiers in the future.
Closing the discussion, LINNC course director Jacques Moret (Bicêtre Hospital, Le Kremlin-Bicêtre, France) described the approach as a “tremendous revolution”—yet one that, as demonstrated in Lylyk’s case presentations, also appears “very simple and very easy” to perform. Moret went on to applaud this innovation—which is the brainchild of neurosurgeon Luis Savastano (University of California San Francisco [UCSF], San Francisco, USA)—noting: “It is based on an idea. It’s the idea that has completely changed the concern of subdural haematoma, and it shows that human intelligence is still extremely important in the development of our field.”