By reprogramming existing spinal cord stimulation systems, investigators have been able to restore efficacy in patients who have failed spinal cord stimulation therapy, and for whom the traditional route would be towards explantation. The results of high-density spinal cord stimulation in failed back surgery syndrome patients were presented by Frank Wille (Diakonessen Hospital, Utrecht, and Academic Medical Center, Amsterdam, Netherlands) at the Annual Meeting of the Neuromodulation Society of the United Kingdom and Ireland (NSUKI; 6–8 November, London, UK).
Explaining the rationale of reprogramming, Wille said, “Everyone who is doing spinal cord stimulation has patients who have failed their therapy over time. But some people, and you cannot predict which ones, lose the effect of their therapy in a couple of months or in a couple of years, and they still have conventional paraesthesia in that area, but they do not have pain relief. Usually these patients get explanted in a couple of months or in a couple of years. In 2010 and 2011, when we had these experiences, we began debating what to do with them— should we explant them and give them an alternative system? What we did first was we tried to reprogramme their existing systems in the same way as this new spinal cord stimulation therapy. From 2011 on, we took all our patients who came in with loss of therapy or with ongoing unwanted stimulation and we started to reprogramme them. We applied the principles of alternative spinal cord stimulation on the existing Medtronic systems.”
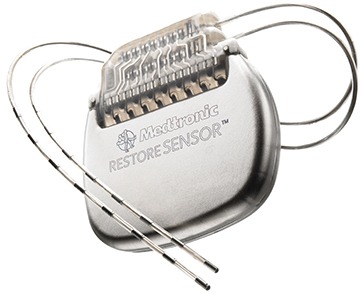
He said that they reprogrammed the stimulation so that it was now high-density, rather than conventional. “We tried to place as close as possible to the T9–T10 target, we applied bipolar electrode configuration, we used maximum frequency which was possible with the already implanted devices and the majority of patients had devices with a maximum of 130Hz or 1000Hz. What is different [from alternative therapy such as high-frequency stimulation] is that we kept the pulse rate as broad as possible, rather than narrowing it. Lastly, we adjusted the amplitude to make it possible to stimulate these patients 24/7,” Wille explained. They then gave the patients trials that lasted at least three days per programme.
After one year, Wille reported, 65% of these patients were still using their spinal cord stimulation system, which Wille said is the most important message. “You can really make a difference for these patients whose only other alternative was to be explanted,” he pointed out.
In terms of what makes the therapy work, Wille said that he believes that is the change in frequency, combined with anatomical target and the fact that the stimulation is continuous.
“In summary, in failed back surgery syndrome patients we showed that high-density stimulation can restore efficacy in failed spinal cord stimulation therapy. It might be superior to conventional stimulation, but a lot of research should be done to evaluate that. In our experience, it is equally effective as the other alternative spinal cord stimulation modes. Maybe all these alternative spinal cord stimulation modes are variations on the same theme, but all of these variations are options for back pain,” Wille maintained.









