Flying a stroke specialist by helicopter to a nearby stroke patient for emergency care is feasible, saves money and, most importantly, gets critical care to patients faster than transporting the patient to a hospital first, according to a single-patient, proof-of-concept study by a Johns Hopkins Medicine research team.
Although the study was not designed to show whether “helistroke service” would improve outcomes for patients, previous research has amply demonstrated that stroke victims do best when they are treated as quickly as possible—ideally in 100 minutes or less.
A report of the findings, published in the Journal of Neurointerventional Surgery (JNIS), details what is believed to be the first test of transporting a physician by helicopter to perform a standard intervention for a stroke.
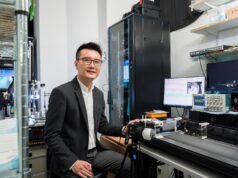
“With the development of effective treatments, the most limiting factor to treating acute stroke is infrastructure—we have to keep evolving our systems to get therapy to as many appropriate patients as possible,” said Ferdinand K Hui, associate professor of Radiology and Radiological Science at the Johns Hopkins University School of Medicine, Baltimore, USA. Hui, the report’s first author, is the physician who was transported via helicopter for the study.
In the traditional model of care, people experiencing an acute ischaemic stroke are taken to a hospital with a specialised centre capable of providing thrombolysis or thrombectomy.
Patient transport time, however, can be significant and, in many cases, stroke victims are first taken to a nearby community hospital, then transported to the specialised centre, often further delaying time to treatment and lowering the odds of recovery or reduced disability.
In a recent study analysing the results of a global, multicentre trial, data show a 91% probability of favourable stroke outcome if patients’ blood flow was restored within 150 minutes of stroke. The next 60 minutes of delay, researchers found, resulted in a 10% reduction of good outcome. An additional 60 minutes resulted in an additional 20% reduction of good outcome. For the best chance of a favourable outcome, preintervention time was calculated to be less than 100 minutes.
To test the feasibility of a physician-to-patient model that could potentially improve outcomes for a time-sensitive procedure, investigators designed a study to fly Hui by Johns Hopkins Lifeline helicopter from Baltimore to a National Institutes of Health Stroke Center at Suburban Hospital in Washington, DC, USA—39.4 miles away—to treat a stroke victim. Suburban, part of the Johns Hopkins Health System, has radiologists and the necessary equipment to image blood vessels but no neurointerventional experts on hand to provide immediate, catheter-based treatment.
A patient was eligible for treatment in the pilot study if he or she had a large vessel blockage and a National Institutes of Health Stroke Scale (NIHSS) rating greater than 8, which is considered a severe stroke.
In January 2017, such a patient was identified at Suburban at 11:12 a.m. Scans to view the patient’s blood vessels and brain tissue were initiated at 11:46 a.m. and completed at 11:58 a.m.
Hui, who was at the Johns Hopkins Hospital in Baltimore, was alerted at 12:07 p.m. Johns Hopkins Lifeline, which provides critical care transportation, was called at 12:13 p.m. Weather clearance for helicopter takeoff was obtained at 12:24 p.m., and the helicopter flight from The Johns Hopkins Hospital to Suburban Hospital took 19 minutes.
Hui inserted the catheter into the patient at 1:07 p.m. and completed treatment at 1:41 p.m. Total time between decision-to-treat and groin puncture was 43 minutes, and between decision-to-treat and groin closure was 77 minutes. These times are comparable with time to treatment in one institution without transfer. The patient received IV t-PA and improved clinically.
Hui says the helistroke service model not only has the potential to reduce transport time and improve patient outcomes, but also could expand ideal standards of care to rural and other populations, where specialised care is limited.
“Up until now, the model has been that the ‘right place’ was a central location, like a tertiary facility such as the Johns Hopkins Hospital,” said Jim Scheulen, chief administrative officer of Emergency Medicine at the Johns Hopkins Hospital. “But what we have demonstrated here is that bringing the right resources in the right time to the patient may actually be a better approach than always moving the patient.”
Hui cautioned that the helistroke service is not always the right or best choice: weather restrictions, specialist availability and transportation costs limit the use of the model. But flying a specialist to a patient may also eliminate some costs of nursing care, monitoring equipment, and the costs of ambulance services to one or more hospitals, as well as potentially fewer days of hospitalisation and rehabilitation for stroke patients, he said.
Although costs vary among regions and hospital networks, the cost of transferring a physician in this case was roughly 20% (US$2,000–US$3,000) of the average patient helicopter transfer cost (US$6,500–US$8,000) for the hospital network.
Other authors on this paper include Amgad El Mekabaty, Kelvin Hong, Karen Horton, Victor Urrutia and Shawn Brast of Johns Hopkins Medicine; Jacky Schultz of Suburban Hospital; and Imama Naqvi, John K Lynch and Zurab Nadareishvili of the National Institutes of Health.