Mission Thrombectomy 2020+ (MT2020+), a global campaign of SVIN (Society of Vascular and Interventional Neurology), recently published Mechanical Thrombectomy for Acute Stroke. Building Thrombectomy Systems of Care in Your Region: Why and How—a white paper targeted towards health policymakers. The paper examines the widespread inaccessibility and geographical disparities in receiving mechanical thrombectomy, and calls for sweeping increase in awareness, accessibility to thrombectomy, and action on a worldwide level.
SVIN notes that currently, the US is a global leader in mechanical thrombectomy use, but that the burden of care is almost four to five times greater in many lower- to middle-income countries. According to MT2020 (now re-named MT2020+ due to ongoing work into 2021 and beyond), the data on stroke patients and the level of care they receive are as follows.
- Each year, approximately 13.67 million people suffer from strokes worldwide
- 20–30% of all ischaemic stroke cases are due to a large vessel occlusion stroke, which makes them eligible for mechanical thrombectomy
- Less than 10% of eligible large vessel occlusion stroke patients receive thrombectomy, leaving approximately two million people in need for this procedure but unable to receive it.
One of the main goals set forth by the initiative and detailed in the report are to implement public health interventions to double global access to mechanical thrombectomy every two years for the next decade.
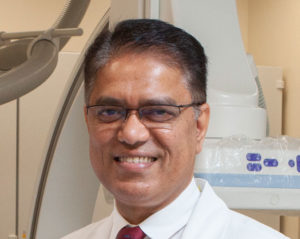
Dileep Yavagal, Global Chair MT2020+ and Global Executive Committee (GEC) co-chair and past-president of SVIN, points out that the campaign is well on its way to increasing the annual rate of stroke thrombectomy for eligible patients to 202,000 annually by the end of last year. “Large vessel occlusion stroke is a longstanding silent global crisis that now has a highly-effective solution since the last five years: mechanical thrombectomy. However, thrombectomy care is not widely accessible with colossal geographic disparities on a global level,” said Yavagal, “We are calling on public health policymakers to increase physical, financial and diagnostic access to thrombectomy for patients with disabling stroke to prevent a lifetime of suffering and death.”
The white paper also provides perspective on:
- Cost-effectiveness of patient care afforded by successful implementation of mechanical thrombectomy protocols
- Tracking metrics and analytics made available through the dedicated MT2020 Global Thrombectomy Tracking (GTT) app
- Educational tools for members of the community
- Training initiatives for EMS and healthcare professionals
- Building thrombectomy systems-of-care in the community
- Improving inter-hospital transfers for mechanical thrombectomy patients
The white paper will be disseminated in six continents with the long-term goal being widespread availability of mechanical thrombectomy as the standard of care globally.
SVIN held its GEC meeting in Los Angeles, USA, in early 2020. MT2020+ members presented country- and region-specific analyses of stroke care. These highlight where stroke care is currently positioned in these countries, roadblocks, and how change can be achieved.
India
P N Sylaja (professor of Neurology, and head of the comprehensive stroke care programme in Sree Chitra Tirunal Institute of Medical Sciences and Technology, Kerala, India) presented an update on the access to stroke care across India.
The presentation began with different stroke registries across India. The Trivandrum Stroke Registry showed an incidence of 135 strokes per 100,000 members of the population, with 74.8% of those being ischaemic, and 14.3% being haemorrhagic; in the Ludhiana Stroke Registry, there was an incidence of 162.3 strokes per 100,000 people with 73% of those being ischaemic, and 25.7% haemorrhagic. Finally, the Kolkata Stroke Registry recorded an incidence of 145.3 strokes per 100,000 people, with fatalities reported at 41.08% after 30 days.
An important takeaway was that in rural areas, there are higher rates of fatality related to stroke. In the Trivandrum Stroke registry, the rate of fatality after 28 days was 37.1% in rural cases, compared with 24.5% in urban. According to Sylaja, one barrier regarding the access to stroke care in India is transport, not just in rural areas but also in cities. “Poor availability of transport in rural areas and congestion in urban areas are barriers to immediate hospitalisation and initiation of treatment.” In a study lead by Sylaja herself, published in Stroke in January 2018, it was found that only 1.8% of stroke patients were brought to hospital by paramedics, while 52% used private transportation.
According to Sylaja, a factor in access to rapid treatment is a lack of education about, and understanding of, stroke symptoms. Further, the Indian population often looks towards alternative medicines for the treatment of stroke. This finding was borne out in the results of a study published in Topics in Stroke Rehabilitation in 2012, which looked at complementary and alternative medicines used in stroke treatment in India. Forty six per cent of stroke patients studied were found to use Ayurvedic medication, 15% intravenous therapies, and 11% used herbal medication.
Latin America
Santiago Ortega-Gutierrez (director of Neurointerventional Surgery, associate clinical professor of Neurology, Neurosurgery and Radiology at the University of Iowa, Iowa City, USA, and global vice chair of MT2020+) next presented data on stroke care in Latin America.
Over the last three years Ortega-Gutierrez reveals that dedicated efforts to collaborate with different regions in Latin America and help with stroke education and systems development, primarily in Peru, Ecuador and Argentina, have been undertaken.
According to data he presented, many South American countries do not have a national plan for stroke, with the exception of Brazil and Chile. According to Ortega- Gutierrez, the main barriers to stroke care across Latin America include: lack of awareness of stroke symptoms, stroke not being treated as a priority, delays in arrival and transfers, lack of well-established transport, poorly established stroke policies, many hospitals being improperly prepared for stroke care, crowded public hospitals, limited funding, and limited neurointerventional training. Moreover, Ortega-Gutierrez stated that the ethnic and socioeconomic disparities are very pronounced.
Ortega-Gutierrez remains optimistic that things could change rapidly. He points to Brazil’s success following the RESILIENT trial, which demonstrated the benefit of mechanical thrombectomy in Brazilian public hospitals, which was used to convince the government to change its policies. “This exemplifies that Latin America has an exceptionally passionate group of physicians, that when provided with adequate resources, can improve stroke care and overcome then care barriers,” he says.
Africa
Mehari Gebreyohanns (Department of Neurology, University of Texas Southwestern, Dallas, USA) presented on the current state of stroke care across Africa and saw the main problems as being the “extreme” lack of resources, and a concentration of available resources within the cities.
Gebreyohanns reflected on some of the barriers that could hinder the progress in stroke care across the continent. Importantly, one of the first stumbling blocks is that there may be no specific medical vocabulary in the African languages (of which there are an estimated 2,000 in the continent) for stroke. Secondly, there is a significant shortfall in the number of neurologists, with only one for every five million people, and these are concentrated in the capital cities. The systems of care too are not well developed, Gebreyohanns said, illustrating that these include emergency medical services, emergency room triage, and the existence of dedicated stroke units and protocols. Thirdly, there is a lack of availability of drugs, especially of tissue plasminogen activator (tPA). Then, there is a lack of what Gebreyohanns described as “basic” equipment, including CT scanners, MR imaging, and catheter labs, which are only available in a few big cities.
Despite these large roadblocks, Gebreyohanns pointed to signs that things may improve including the creation of a word for stroke in the Ethiopian language, which would translate to “brain attack”. Other positive developments include programmes run by the Bahir Dar Outreach for Neurology Education (BORNE) initiative, which he founded, that aim to improve the state of stroke care with Bahir Dar University in Ethiopia. Gebreyohanns says this initiative includes institutional relationship building, global neurology elective courses for residents, yearly teachings and symposia, skills training and cross-training, telemedicine, and web-based skills training.
Middle East and North Africa
Ossama Yassin Mansour (professor of Clinical and Interventional Neurology, Stroke and Neurointervention services at Alexandria University, Egypt, and president of Middle East North Africa Stroke and interventional Neurotherapies Organisation [MENA-SINO]), presented the Middle Eastern and North Africa perspective.
The Middle East and North Africa (MENA) region encompasses 17 countries, with an estimated population of 578 million. Mansour commented: “In the absence of good quality data on stroke incidence and prevalence from the region, the exact burden of this devastating disease is hard to determine. However, the MENA region has a relatively young population, with more than 40% of the region’s population being below 15 years of age and just 4% being over the age of 65, indicating that in the future, the impact of stroke will become an increasingly huge burden.”
Mansour reported that the incidence rate for all strokes ranged between 22.7 and 250 per 100,000 population per year. There was a 75% high male-to-female ratio among stroke patients, and the age of a stroke incidence was typically in the sixth, or seventh decade. Mansour cited a prospective observational hospital study from Qatar, where only 17.5% of ischaemic stroke patients arrived in hospital within three hours of stroke onset. He also referenced a prospective study conducted in the Neurology Department of Istanbul Medical School in Turkey, where the admission of stroke patients is dependent on the availability of beds.
Mansour described the stroke care system across the region as “in its infancy”, and, noted that, despite strides in the last two decades, there are still too few centres providing intervention. “To the best of our knowledge, before 2012, there were fewer than ten centres that were treating patients with intravenous thrombolysis for acute ischaemic stroke in the whole region, and the rate of thrombolysis was less than 1%.”
Mansour concluded by showing that there has been some growth in stroke care across the region achieved through the MENA-SINO, which began in 2013 with a group of strokeologists and neurointerventionalists coming together to improve ischaemic and haemorrhagic stroke services in the region. The organisation is raising awareness regarding stroke risk factors and identifying the interventions needed; providing education, endovascular thrombectomy training and awareness for stroke care providers; conducting research focused on pragmatic and locally-relevant solutions for reducing stroke burden; building networks of political and professional allies; and disseminating relevant knowledge.
Beyond 2020
In an exclusive interview Yavagal gave to NeuroNews, on MT 2020+, he notes, “The next steps are very exciting, and we have much work to do.”
According to Yavagal, the number of SVIN’s regional committees is expected to grow to over 100. Existing regional committees are currently developing their top five interventions for 2021. “Each region needs a slightly different intervention, for example, educating pre-hospital personnel to recognise stroke is a big requirement in low- and middle -income countries.”
Yavagal also emphasises that a more equitable global access to mechanical thrombectomy rests on the huge task of properly training the medical personnel needed to perform mechanical thrombectomy, which is closely linked to the set-up of stroke centres around the world.
Yavagal left with this comment, “multiple stakeholders from every aspect of public health need to come together, along with policy makers and governments, to advance MT 2020+ because, we finally have a very important treatment that actually reduces the disability from stroke. Without a global implementation of this powerful treatment, the benefit will not be realised in any good measure.”