This advertorial is sponsored by WallabyPhenox.
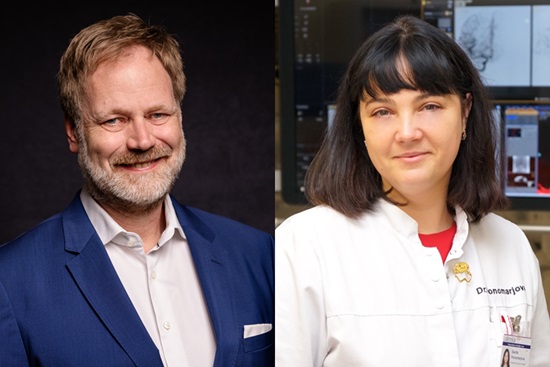
While the endovascular treatment of intracranial aneurysms has evolved substantially in recent times and a plethora of novel technologies have been introduced, coil embolisation remains the most commonly used modality across the globe and at many centres. As such, continued innovation and updates to coiling systems therefore bring with them major implications for neurointerventionalists as well as their patients. Here, Jan Höltje (University Hospital Schleswig-Holstein, Lübeck, Germany) and Sanita Ponomarjova (Riga Eastern University Hospital, Riga, Latvia) share their experiences as two of the first physicians in Europe to perform brain aneurysm treatments using the latest advancement in coiling: the Avenir Pico system (WallabyPhenox).
Perhaps the most pertinent appraisal of Avenir Pico comes from Höltje and Ponomarjova’s parallel responses when asked if they would recommend this newly available coil to their peers in the neurointerventional space, with both simply answering: “Yes, absolutely.”
The two highlight broadly similar advantages based on their initial experiences with the device, including its ability to successfully find and fill spaces within the neurovasculature while also maintaining its shape. Avenir Pico’s softness and flexibility, as well as its simple yet effective detachment system, are among other positive characteristics called out by both physicians.
First-time success
Speaking to NeuroNews, Höltje notes that he will often favour a coiling-led strategy for the majority of small-neck aneurysms, and also wide-neck aneurysms in which an intrasaccular system is less likely to perform well, such as those with more irregular or complex shapes. And, while their usage has diminished somewhat in recent years, he feels coils remain a “very important device” in aneurysm care.
“I was already aware of the original Avenir coils—and I always like to try new things!” says Höltje, detailing that he was first introduced to the more novel Avenir Pico system at the 2025 European Society of Minimally Invasive Neurological Therapy (ESMINT) annual congress (3–5 September, Marseille, France), subsequently acquiring it at his centre and debuting it in a clinical case the following month.
The case within which Höltje has used Avenir Pico to date involved a patient with an unruptured, small-neck aneurysm located in their internal carotid artery (ICA). On this point, he comments that, “there are always other ways but, for me, coiling is clearly the best way to treat this type of aneurysm”.
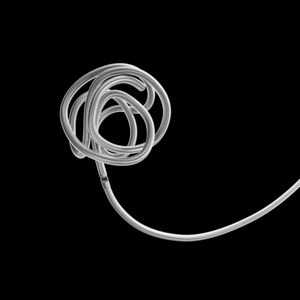
Reflecting on said first case, he highlights the Avenir Pico coil’s softness, the packing volume he was able to achieve, and a “really simple and safe” detachment mechanism, as the most noteworthy aspects of the treatment—also noting that he occluded the aneurysm without leaving behind any neck remnants, and without the need for any adjunctive devices. The patient ultimately experienced a positive clinical outcome and returned home the day after the procedure.
“It worked exactly as I had hoped and everything was precisely how a coil should work,” Höltje avers. “I was a little bit sceptical of the detachment system [beforehand], but it worked really well.”
He also states that Avenir Pico’s pair of radiopaque detachment markers meant he was able to clearly visualise the coils staying in place and the delivery wire being retracted successfully during the procedure—whereas, with certain other devices, it can be “very hard” to see the delivery wire, thus creating a degree of uncertainty for the operator.
Höltje adds that, overall, Avenir Pico has a relatively minor learning curve, and therefore represents a “good choice” for any clinician performing their first coiling procedures, once again citing the simplicity of its detachment mechanism and the broad range of available device sizes—62 in total—as prominent strengths of the system.
Acute and elective uses
Ponomarjova initially notes that the configuration of an aneurysm’s neck is likely to be the single biggest anatomical factor that influences her selection of an endovascular approach. She also tells NeuroNews that, in her practice, she prefers to use coiling rather than intrasaccular remodelling, as the former technique allows her to be more adaptable if multiple attempts or retreatments are required, while the ability to deploy supportive devices like the pConus bifurcation aneurysm implant (WallabyPhenox) opens up an even wider array of treatment options.
The first of two cases within which she has utilised Avenir Pico to date involved an 80-year-old patient with an irregularly shaped wide-neck aneurysm—located in the middle cerebral artery (MCA)—who was adjudged to have a high rupture risk. Ponomarjova relays that she used the pConus device to protect the neck of the aneurysm.
“I was very nicely surprised and impressed because, although the pConus’ position in the aneurysmal sac was a little bit deeper than I was expecting, the Avenir Pico coil kept its shape really well,” she recalls. “It was also really nice to see how well the coil packing was performed.”
Ponomarjova’s second Avenir Pico treatment was an acute case involving another elderly patient—this time with a ruptured MCA aneurysm. She comments that treatment decision-making proved especially complicated due to the aneurysm in question featuring two distinct lobes, with the larger one having a “very wide” neck.
Ponomarjova therefore embolised the lobes separately, and found that the Avenir Pico coil maintained its shape without any protrusion inside the arterial lumen, remaining securely inside the sac and producing no thrombogenic complications while also demonstrating an impressive level of packing density. She attributes this last observation to Avenir Pico’s softness and flexibility, and compliments its stability within the aneurysm neck, also emphasising the benefits of a coil that can “squeeze” into more confined locations within the neurovasculature while retaining its structure. In Ponomarjova’s view, the ‘shape-memory’ quality of the device coupled with its conformability is a particularly advantageous combination in ruptured cases, during which the consequences of asserting too much pressure on the aneurysmal wall are more severe.
“These are really important features,” she adds. “The coil showed a very good performance, because the aneurysm shape was not simple, and I was quite concerned about occlusion of the branch—but it worked really well.
“The detachment system is very reliable too. It is mechanical rather than electrical, so—once you have done all of the correct steps—you can be completely sure that the coil has detached, which may be especially important in smaller aneurysms where there is a greater risk of losing the position of your microcatheter. As such, I think it is a good choice for younger doctors who have less experience to start with this highly reliable coil.”
Ponomarjova reports that the first of these two patients achieved a good clinical outcome after the procedure and left the hospital three days later, while the second returned home “in a very good condition” after two weeks, having been monitored for longer due to her initial presentation with subarachnoidal bleeding.
“There are quite a lot of coils now available to us on the market, so it is often difficult to find the small nuances between them,” she comments. “But, for me, the Avenir Pico is very good at finding space easily and finding the best spot, with minimal friction, meaning you can achieve better packing. This is especially important when you are using combined remodelling techniques involving balloons or stents.”
Future directions
A final point on which the two physicians are in agreement is the fact that, beyond intracranial aneurysms, there are several further indications that the Avenir Pico coil could prove useful for in the future.
Ponomarjova highlights minimally invasive embolisation for head and neck tumours, as well as the current ‘hot topic’ of middle meningeal artery embolisation (MMAe) in chronic subdural haematoma (cSDH) patients, as potentially promising areas, while Höltje sees a possible role for Avenir Pico in ‘pressure-cooker’ techniques used to treat brain arteriovenous malformations (AVMs) and to halt bleeding in patients referred for endovascular therapy by ear, nose and throat (ENT) surgeons.
CE-mark approval and a European limited market release of the Avenir Pico coil system were announced by WallabyPhenox in November 2025—with the device having already seen rapid adoption across the pond following its US Food and Drug Administration (FDA) clearance several years ago.









