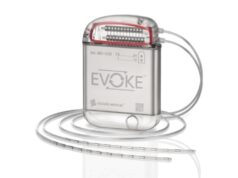
New data from both the Evoke and Avalon studies reiterate the importance of objective neurophysiological measures and clinically meaningful outcomes. These studies evaluated the performance of the first closed-loop spinal cord stimulation (SCS) system (Evoke; Saluda Medical) that objectively measures the spinal cord’s response to stimulation and both studies have in turn demonstrated improvements in pain, function, sleep, and quality of life.
“For the first time, we use physiology to guide our decisions. When employing evoked compound action potentials [ECAPs] to control a feedback mechanism—providing more precise spinal cord activation—the results elicit superior clinical outcomes,” surmised Lawrence Poree (University of California, San Francisco, USA) while presenting the Evoke study during the International Neuromodulation Society (INS) 14th World Congress (25–30 May, Sydney, Australia).
The Evoke study is a prospective, multicentre, randomised, double-blind pivotal study comparing ECAP controlled closed-loop SCS with open-loop (fixed output). Providing the rationale behind the novel Evoke System, Poree put forward, “We know that the epidural space is a dynamic environment, and that the region of the spinal cord that is targeted may not always receive the stimulation we program as the spinal cord position within the electric field is constantly in motion due to cardiac pulsations, respiration, coughing, positional changes and so on. At this time, commercially available spinal cord stimulation devices are incapable of detecting and accommodating for most of these variables.”
Ultimately, Poree stated that the primary question that needed answering was whether analgesia and other patient quality of life measures could be improved using an individual’s evoked compound action potentials to control the output of the SCS device in a closed-loop fashion.
Providing further explanation, he said, “Every individual patient has an individual ECAP signal that corresponds to their pain control. This represents their therapeutic window, the threshold, the maximum, and the comfort level. Once this therapeutic window is set, then the decision is made as to whether the patient will make all the adjustments to the stimulator to maintain the appropriate current output to maintain optimal analgesia (open loop) or if the primary control is turned over to the computer in the SCS implantable pulse generator to maintain a constant ECAP response (closed-loop) in much the same way automobiles equipped with cruise control can maintain a constant speed regardless if the vehicle is going uphill or downhill.
“When we give it to the computer, it uses that information in real-time to feedback and decide whether the output of the device should be lower or higher depending on the precise response of the individuals evoked compound action potential immediately before each stimulus,” Poree noted.
In terms of the study’s methodology, he said that an important aspect was that the ECAPs were collected and analysed in all patients, not only those receiving closed-loop stimulation and the in-office programming to determine the individual therapeutic window was the same for both the open and closed loop groups. In addition, he highlighted that the decision about which group each patient was being allocated to was made after the surgical placement of the leads and determination of the therapeutic window.
“The primary objective was to demonstrate non-inferiority, and then test for superiority. The endpoint was a 50% reduction in overall trunk and limb pain as determined by VAS,” said Poree. Describing the characteristics of the population, he noted that overall, around 63% of patients in both groups were taking opioids. Ages were similar, as well as duration of pain; between 11 and 13 years, and pre-operative VAS scores were the same.
Moreover, Poree emphasised that a variety of other measures were kept constant between the groups, such as the programming time of the patients and frequency range and pulse width. Additionally, lead location and the length of the trial were also kept constant.
Also presented at the INS World Congress were long-term data from the Avalon study. Charles Brooker (Royal North Shore Hospital, Sydney, Australia), one of the study’s principal investigators, revealed the 18 month outcomes from this Australian prospective, single-arm study. As the effective relief of pain and associated symptoms were weighed against the same system, Evoke, the findings from both studies are outlined below.
Evoke and Avalon: The findings
The key three-month results of the Evoke pivotal study include how the closed-loop arm met all the pre-specified endpoints, and demonstrated statistically superior back and leg pain relief (with no increase in pain medications) compared to controls, with over 80% (82.5%; 51/62) of closed-loop subjects achieving greater than or equal to 50% pain relief (control: 60.3%; 38/63).
Furthermore, Poree reported that more than half of closed-loop subjects (58.1%; 36/62) were high responders, as they achieved greater than or equal to 80% reduction in back and leg pain (control: 42.9%; 27/63). In addition, the investigators observed that closed-loop maintained spinal cord activation within the therapeutic window 1.5 times that of the control group (91.1% of the time with closed-loop vs. 59.5% for controls).
The findings from the Avalon trial only reiterate these successful outcomes. At 18 months, 69.4% (25/36) of participants implanted with the Evoke system experienced more than 80% pain relief, while 83.3% (30/36) experienced a clinically meaningful improvement in quality of life. Brooker also reported that disability was reduced, with 72.2% (26/36) of patients having only minimal to moderate disability compared to 18% at baseline.
In terms of a reduction in opioid medication, Brooker said that more than two out of three patients (67.9%; 19/28) reduced or eliminated their intake in the Avalon study, and lastly, he told the INS audience that spinal cord activation was maintained within the therapeutic window 97.5% of the time.
In light of these findings, Brooker told the INS, “With Evoke, study results suggest that pain relief continues to improve over time, which is not typically observed with fixed-output systems. With the capability of neurophysiology measurements, such as percentage time in the therapeutic window, we can now start to understand a complex condition objectively in addition to patient reported outcomes, an important advancement to the field of pain management.”
Furthermore, Steven M Falowski, director of functional neurosurgery at Neurosurgical Associates of Lancaster (Lancaster, USA), and an investigator in the Evoke Study, commented on the data, “Both studies provide evidence supporting the novel design of the device where ECAPs are measured to monitor therapy delivery in real time. The technology provides an objective measure based on a neurophysiological response to control therapy delivery and provides insight into the mechanism of action. There were a plethora of talks featuring ECAPs at this congress and they highlight the potential clinical utility of this new technology.”