The neuromodulation space has proliferated significantly over the past few years, and one area in which this is most notable is with the expansion of spinal cord stimulation (SCS)—not only in terms of technological advancements, but also regarding the gamut of conditions it is used in. Here, Todd Bromberg (Chalfont, USA) takes a closer look at how SCS is impacting the treatment of a currently underserved group of diabetes patients.
In patients with diabetes, high serum glucose levels can lead to damage of the peripheral nerves—a condition known as diabetic peripheral neuropathy (DPN). DPN can be painful and debilitating, and patients with painful DPN can experience numbness, and burning or stabbing sensations in areas surrounding affected nerves, most often in the legs and feet. This can negatively impact quality of life, making it difficult to ambulate and sleep, and numbness can lead to additional health complications. Loss of sensation may also allow cuts or sores in the feet to go untreated, potentially leading to infections that may become life-threatening and/or require amputation.
The first step in managing/preventing painful DPN is helping patients maintain and achieve strict glucose control. Beyond this, traditionally there have been four approaches to managing symptoms: medical management with pharmaceuticals; non-pharmacological options, such as sympathetic nerve blocks; mental health interventions, including psychotherapy to help address the mental health impacts, cognitive-behavioural therapy, and biofeedback; and alternative therapies, such as acupuncture and hypnosis.
Neuromodulation comes to the fore
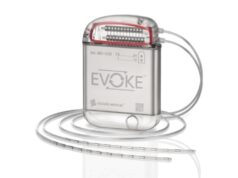
More recently, SCS has been approved for the treatment of painful DPN. SCS is a form of neuromodulation that applies electrical impulses to targeted areas of the spine in order to modulate, or change, how those pain signals communicate pain to the brain. SCS has a long track record for treating chronic low-back and leg pain, and extending this therapy to the treatment of DPN follows decades of safe and effective use for other medical conditions. In SCS, stimulation is delivered to the spinal cord using a neurostimulator, which is a small device similar to a pacemaker that is implanted under the skin. The electrical impulses travel from the device to the spine over thin, insulated wires called leads. The mild electrical impulses delivered by the neurostimulator interrupt the pain signals between the spinal cord and the brain, helping to alleviate pain.
Prior to device implantation, patients undergo a temporary trial for 3–10 days with an external neurostimulator to determine their response to the therapy; patients who experience benefit (≥50% pain reduction) have the option of proceeding to implantation. Once the device is implanted, the patient’s physician will help adjust the settings to achieve optimal pain relief. The development of novel waveforms in recent years—such as differential targeted multiplexed therapy (Medtronic)1, burst therapy (Abbott)2, and high-frequency therapy (Nevro)3—enables customised treatment that can provide highly personalised pain management.
Implantable SCS devices have been used for the treatment of chronic pain since 1981. Over the past 40-plus years, continued innovation in SCS technology has enabled the use of smaller devices, and has produced novel algorithms that allow treatment to be tailored to each patient’s unique pain profile. Today’s SCS devices come in rechargeable and recharge-free formats, making it easier for patients to find a system that works best for their needs and lifestyles. Some systems allow magnetic resonance imaging (MRI) access under certain conditions, which obviates the need to remove the device if patients need to undergo an MRI after they have started SCS therapy. Mobile applications are also available with some SCS devices, which can help keep patients informed and connected to their care teams while they undergo SCS therapy.
An established evidence base
SCS has been used successfully to treat chronic pain—primarily in the lower back and leg—for four decades. More recently, however, SCS has been added to the armamentarium of treatments for DPN-related pain. SCS is thought to work for painful DPN in the same way as chronic low-back and upper-leg pain; by modulating pain impulses and blocking pain signals from reaching the brain. The US Food and Drug Administration (FDA) first approved the use of SCS for the treatment of painful DPN in July 2021 and, today, three SCS manufacturers—Medtronic, Abbott and Nevro—have FDA clearance to market their therapies for this condition.
Data from multiple randomised controlled trials (RCTs) show that patients with painful DPN treated with SCS have a 53% reduction in pain at six months compared to 0% in control groups.4-6 Eighty-six percent of patients treated with SCS experienced treatment success after SCS therapy for one year, and more than 50% experienced meaningful pain relief through five years.7 Based on these clinical data, patients with painful DPN are 17 times more likely to experience pain relief if treated with SCS compared with conventional treatments alone.4-6 More than 50% of patients continue to receive clinically meaningful pain relief (>30% reductions in pain) 8–10 years post-implant.9
These clinical findings support the use of SCS in the treatment of painful DPN for patients who cannot effectively manage their pain with conventional medical therapies. Assuring that patients who may benefit from SCS have access to this life-changing therapeutic approach for painful DPN requires collaboration and coordination among multiple care providers. While SCS is a well-known therapy for chronic pain among pain specialists and neurologists, it is less familiar to the podiatrists, endocrinologists, and primary care physicians. It is important for all physicians to become educated about SCS for relieving pain related to DPN. Physicians who implant SCS can facilitate awareness and understanding of this therapy for the treatment of painful DPN by serving as a resource for podiatrists, endocrinologists and primary care physicians in their community.
SCS is an exciting option for helping to improve outcomes for patients with painful DPN. Working together, the medical community can help facilitate adoption of SCS and give more patients the opportunity to achieve effective pain relief. And, with the incidence of diabetes increasing8, it has never been more important for all physicians to remain educated about the treatment options for patients living with DPN.
References:
- Fishman M, Cordner H, Justiz R, et al. 12-month results from multicenter, open-label, randomized controlled clinical trial comparing differential target multiplexed spinal cord stimulation and traditional spinal cord stimulation in subjects with chronic intractable back pain and leg pain. Pain Pract. 2021; 21(8): 912–23.
- Kirketeig T, Schultheis C, Zuidema X, et al. Burst spinal cord stimulation: A clinical review. Pain Med. 2019; Suppl 1: S31–S40.
- Petersen E A, Stauss T G, Scowcroft J A, et al. Effect of high-frequency (10kHz) spinal cord stimulation in patients with painful diabetic neuropathy: A randomized clinical trial. JAMA Neurol. 2021; 78(6): 687–98.
- Medtronic. Medtronic Pain Therapy Clinical Summary M221494A016 Rev B. United States; 2022.
- De Vos C C, Meier K, Zaalberg P B, et al. Spinal cord stimulation in patients with painful diabetic neuropathy: A multicenter randomized clinical trial. Pain. 2014; 155(11): 2426–31.
- Slangen R, Schaper N C, Faber C G, et al. Spinal cord stimulation and pain relief in painful diabetic peripheral neuropathy: A prospective two-center randomized controlled trial. Diabetes Care. 2014; 37(11): 3016–24.
- Van Beek M, Geurts J W, Slangen R, et al. Severity of neuropathy is associated with long-term spinal cord stimulation outcomes in painful diabetic peripheral neuropathy: Five-year follow-up of a prospective two-center clinical trial. Diabetes Care. 2018; 41(1): 32–8.
- World Health Organization. Diabetes: Key facts. Available at https://www.who.int/news-room/fact-sheets/detail/diabetes.
- Zuidema X, et al. Long-term evaluation of spinal cord stimulation in patients with painful diabetic polyneuropathy: an eight-to-ten-year prospective cohort study. Neuromodulation. 30 December 2022. https://doi.org/10.1016/j.neurom.2022.12.003.
Todd Bromberg is a pain management specialist and neurologist at Delaware Valley Pain & Spine Institute in Chalfont, USA.
DISCLOSURES: The author is a consultant for Medtronic, and Medtronic provided technical support for and reviewed the contents of this article prior to publication.