Late-breaking findings from the TWIN2WIN trial—presented recently at the International Stroke Conference (ISC; 7–9 February, Phoenix, USA)—have demonstrated the potential benefits of performing mechanical thrombectomy procedures using two stent retrievers (SRs) simultaneously. The trial compared a first-line dual-SR strategy to a traditional single-SR technique across more than 100 acute ischaemic stroke patients, and found improved recanalisation rates as well as no safety concerns with the more novel of the two approaches.
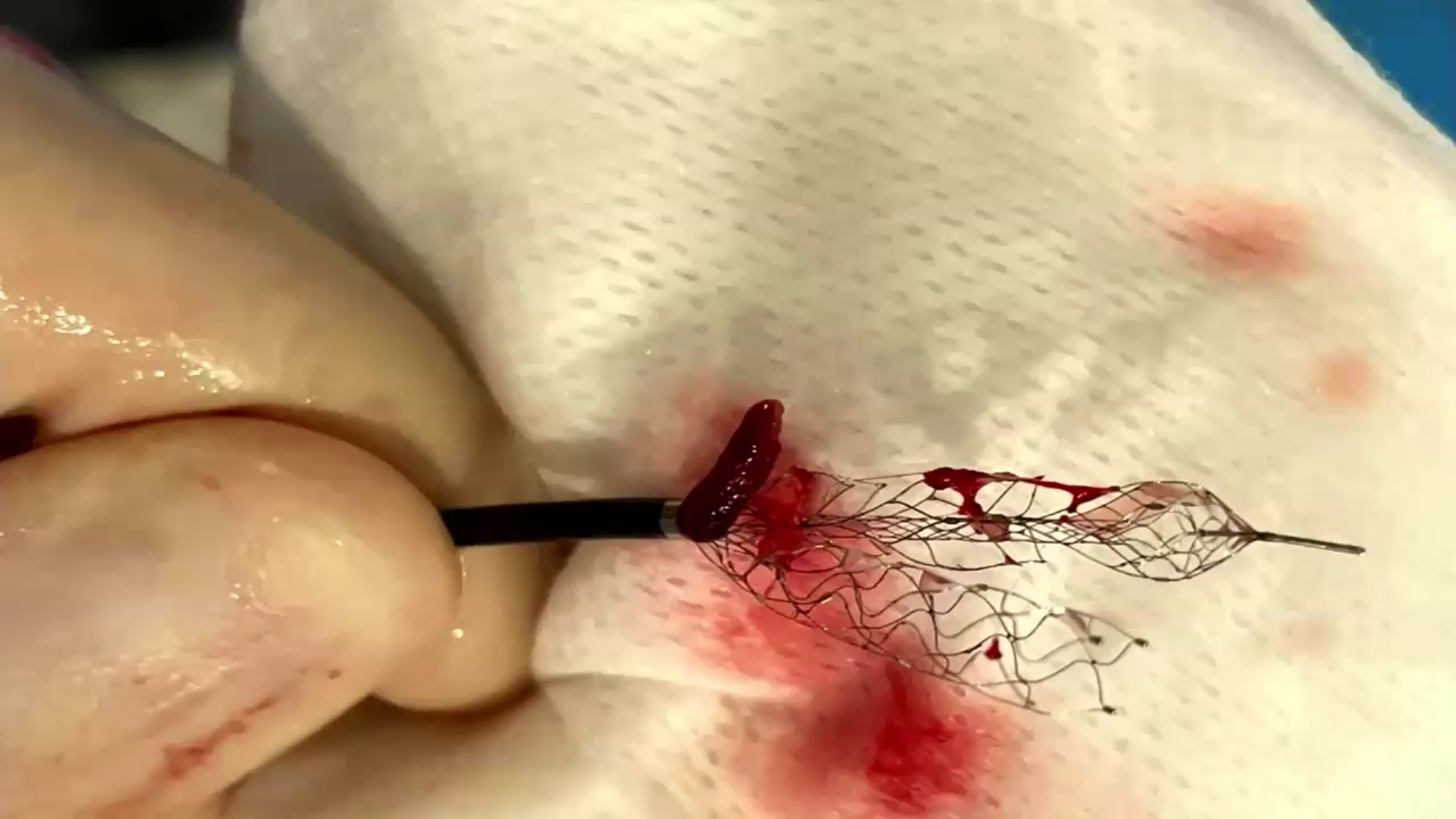
Prior to delivering these data for the first time at ISC 2024, Marc Ribo (Vall d’Hebron University Hospital, Barcelona, Spain) informed the audience that dual-SR techniques have been used for many years as a rescue strategy following initially unsuccessful thrombectomy attempts. He cited the fact that the approach can “dramatically reduce” direct friction between the clot and the arterial wall—instead “sandwiching” the clot between the two device structures—as one of the key benefits of using two SRs.
Recent research has indicated that the concurrent deployment of two SRs could also carry advantages as a first-line thrombectomy technique, particularly in certain middle cerebral artery (MCA) or terminal internal carotid artery (TICA) occlusions, leading to growing interest in this area.
In 2022, Ribo and his colleagues completed an animal study that ultimately suggested one dual-SR thrombectomy pass may induce slightly less cumulative histological damage to the endothelium compared to two passes with a single SR. A later study from Ribo et al involving in-vitro models then revealed positive findings regarding first-pass recanalisation with a dual- versus single-SR approach—a phenomenon found to be more pronounced in MCA occlusions and, in particular, ‘saddle thrombi’ that are sitting across two co-dominant M2 branches.
Considering these two positive signals in combination, Ribo and his colleagues set out to establish a more direct comparison of dual- versus single-SR treatment strategies via the TWIN2WIN clinical trial. This prospective trial enrolled acute stroke patients undergoing thrombectomy—specifically those whose primary occlusion site was a bifurcation located in the TICA, the distal M1 segment of the MCA, or the top of the basilar artery—and randomised them to thrombectomy with either one or two SR devices as the first-line approach. Its primary endpoint was the rate of perfect/near-perfect recanalisation (thrombolysis in cerebral infarction [TICI] 2c–3) at the first pass.
TWIN2WIN was conducted across five clinical sites in Spain, and initially planned to enrol 212 patients. However, according to Ribo, the trial was subject to a preplanned interim analysis after reaching 50% of its intended total patient population in November 2023—and, just a matter of days prior to the deadline for ISC 2024 abstract submissions, received a recommendation from its data and safety monitoring board (DSMB) to stop enrolment due to positive efficacy signals favouring dual-SR thrombectomy in that interim analysis.
Ribo reported that—across the 108 patients who were ultimately analysed—the distribution of occlusion locations was “well balanced”, and there were no major differences in baseline characteristics, between the dual- and single-SR study arms.
As per TWIN2WIN’s primary efficacy endpoint, the first-pass TICI 2c–3 rate was “substantially higher” in the study’s dual-SR arm (46.6%) versus the single-SR arm (24%), with Ribo reporting a statistically significant difference between the two (p=0.015).
Regarding key secondary endpoints, the presenter went on to note “more equal” outcomes in terms of final-pass TICI rates between groups—although there was still a numerically higher rate of TICI 2c–3 recanalisation with the dual-SR approach. He also relayed that, while overall numbers here were low, subanalyses revealed improved rates of successful recanalisation with a dual-SR strategy across different initial occlusion locations, consistent with the primary endpoint finding. Analysis of another secondary endpoint revealed that the mean number of thrombectomy passes was 1.58 in the dual-SR arm and 2.02 in the single-SR arm, while the median numbers of passes were 1 and 2, respectively, in the two groups (p=0.026).
Ribo went on to detail “absolutely no concerns” regarding safety, relaying symptomatic intracranial haemorrhage (sICH) rates of 6.4% in the dual-SR arm and 4.3% in the single-SR arm—both of which, he averred, are “within normal ranges”. He then noted a non-statistically significant trend towards better clinical outcomes in the dual- versus single-SR arm, indicated by average rates of 90-day modified Rankin scale (mRS) scores of 0–1 (12.5% vs. 21.6%, respectively), and also median National Institutes of Health stroke scale (NIHSS) scores at discharge (11 vs. 6.5, respectively).
Finally, Ribo posited that, based on observations in the TWIN2WIN trial, “the duration is not longer with two stents”, owing to average procedure times that were “basically exactly the same”—roughly 45 minutes—in both groups.
“I would conclude that these data show efficacy in terms of angiographic outcomes, and we are already planning further phases to confirm the clinical impact of these results,” he added.









