A study investigating chronic pain sufferers treated with burst spinal cord stimulation (B-SCS) has concluded that improvements were observed among all psychological measures at one year. The largest impact of the therapy was on catastrophizing and depression. “These pain-related beliefs and behaviours, and not pain intensity, have been shown to put patients at greatest risk of a poor prognosis and quality of life,” write the authors, Steven Falowski, Neurosurgical Associates of Lancaster, Lancaster, USA, and colleagues.

Published in Neuromodulation, the study sought to investigate the effect of B-SCS on psychosocial functioning and its influence on pain and quality of life. The rationale of the research pertains to the fact that B-SCS has previously been shown to reduce neuronal firing in the anterior cingulate cortex through selective modulation of the medial pain pathway tract.
Those with chronic, intractable pain of the trunk, and/or lower limbs were eligible for enrolment in the study. Of the 269 patients that were enrolled at 22 centres around the USA, trial success rate was 90%. Once deemed successful, patients received a permanent implant and returned for follow-up at six and 12-months.
Falowski and his team report significant improvements in pain, physical, mental and emotional functioning, observed from baseline to the six and 12-month follow-up (p<0.001).
“Overall, patients had improved quality of life, became more active, and the negative impact of pain on daily life was decreasing,” write the authors. Specifically, at one year, 81% of subjects were satisfied or very satisfied with their therapy. Additionally, subjects showing significant improvements on mental health outcomes reported enhanced pain relief and quality of life scores compared with subjects with continued impaired mental health at follow-up.
Regarding reduced opioid usage, the team found that at one year, 89% of subjects who were taking opioids at baseline decreased, or stayed at the same level of opioid use, and 19% stopped taking opioids altogether.
Discussing the importance of these findings, Falowski et al state that chronic pain affects approximately 30% of adults worldwide, and is constantly associated with psychological disorders across all geographies. “Patients seek medical care for pain, not only for diagnostic evaluation and symptom relief, but also because pain interferes with daily activities, causes worry and emotional distress, and undermines confidence,” they note.
The team also highlights that expanding the literature on quality of life outcomes will provide clinicians with additional data to better educate patients about the benefits of SCS, and set comprehensive goals for treatment outcomes.
Pointing to a particular caveat, Falowski and colleagues acknowledge that as the current investigation is a real-world study, stringent programming and cycling guidelines could not be imposed, even as recent research has demonstrated the benefits of optimising clinical settings for B-SCS.
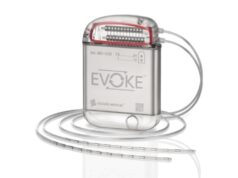
However, they write that because the study had broad inclusion criteria, the internal pulse generator (IPG) systems and electrode configurations were used according to physician preference. “Our study represents real-world outcomes, illustrating the effectiveness of B-SCS to address the affective component of pain in a representative population rather than a tightly controlled environment,” Falowski and team surmise.
Moving the field forward
The team speculates that future research should seek to refine programming and stimulation configurations in the field of neuromodulation.
Speaking with NeuroNews, Falowski comments: “We are moving away from subjective and largely inaccurate pain scores for patients. It is more important to deliver functional improvements and quality of life to our patients.
“This study has shown that not only can we improve pain scores, but we can now truly improve patient outcomes with objective measures that are more correlative to their outcomes. Perhaps the most impactful is that this real world study was able to improve pain catastrophizing in our patients to be in line with or better than a normal population.”