Analyses of a large US registry comparing first-line stroke thrombectomy approaches for medium-vessel occlusion (MeVO) stroke have shown that direct aspiration is associated with significantly lower rates of symptomatic intracranial haemorrhage (sICH) and vessel injury/vasospasm compared with stent retrievers. A trend towards higher rates of excellent 90-day outcomes (modified Rankin scale [mRS] 0–1) with aspiration thrombectomy was also observed, as per a late-breaking data presentation from Shahram Majidi (Mount Sinai Health System, New York City, USA) at this year’s Society of NeuroInterventional Surgery (SNIS) annual meeting (14–18 July, Nashville, USA).
Majidi and colleagues’ analysis evaluated all MeVO stroke patients treated via thrombectomy within the large, nationwide NeuroVascular Quality Initiative-Quality Outcomes Database (NVQI-QOD) acute ischaemic stroke registry from 2014–2025, with MeVOs being defined as occlusions at or distal to the following locations: the M2 segment of the middle cerebral artery (MCA), the P1 segment of the posterior cerebral artery (PCA), or the A1 segment of the anterior cerebral artery (ACA). Patients were allocated to either the aspiration cohort or the stent retriever cohort based on the initial, first-line treatment technique they received.
According to Majidi, key efficacy outcomes of this research included rates of successful recanalisation, time from access to recanalisation, excellent (mRS 0–1) and favourable (mRS 0–2) clinical outcomes at 90 days, and mortality at 90 days, while procedure-related occurrences of all ICHs, sICH and vessel injury/vasospasm were the main safety-related outcomes of interest.
A total of 3,059 stroke patients with primary MeVOs were identified, and the researchers found that 48% had been treated via a direct aspiration-first approach compared to 52% being treated using stent retriever-first techniques. Patient sex, median age and relevant comorbidities were all comparable between these two groups. The M2 segment of the MCA constituted the most common primary occlusion location in Majidi and colleagues’ analysis, at a frequency of more than 80% in both groups, while femoral access was preferred over radial access in the majority of cases—although radial access was selected more regularly in the aspiration cohort (17.3%) compared to the stent retriever cohort (9.9%).
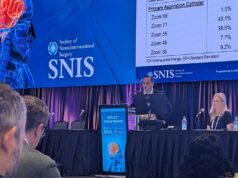
The analysis’ efficacy outcomes found that, while first-pass modified thrombolysis in cerebral infarction (mTICI) 2b–3 and 2c–3 rates were statistically similar between the two patient cohorts, those treated via an aspiration-first approach achieved a higher average rate of complete recanalisation (mTICI 3) compared to their counterparts who underwent first-line stent retriever thrombectomy (25.3% vs 21.1%, respectively). Additionally, final recanalisation rates—defined as the patient’s mTICI score after all thrombectomy passes have been completed—were statistically significantly higher with first-line aspiration versus stent retriever treatment for both mTICI 2c–3 (58.4% vs 53.9%), and mTICI 3 (44.5% vs 39%). Majidi and colleagues also found that total procedure durations—defined as time from groin puncture to final reperfusion—were very similar between groups, at 28 and 29 minutes, respectively.
Clinical outcome assessments from the analysis revealed a trend towards improved rates of 90-day mRS 0–1 and mRS 0–2, at 52% and 65% in the aspiration group versus 47% and 61% with stent retrievers, but Majidi relayed that no statistically significant discrepancies were observed—and the same rate of mortality at 90 days (7%) was seen in both groups too.
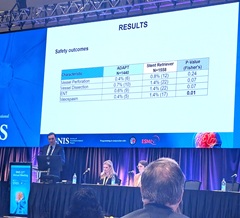
Moving on to disclose the analysis’ main safety outcomes, the presenter reported a statistically significant reduction in the rate of any ICH on 24-hour computed tomography (CT) imaging within the aspiration group (24%) compared to the stent retriever group (31%), as well as a decrease in sICH rates—as per the European Cooperative Acute Stroke Study (ECASS) II definition—with aspiration (5%) versus stent retrievers (8%). Majidi further detailed that, “as expected”, rates of subarachnoid haemorrhage (SAH) and intraventricular haemorrhage (IVH) were lower in the aspiration cohort (7% and 0.5%, respectively) compared to the stent retriever cohort (14% and 1%, respectively).
An additional four safety-related measures were evaluated in Majidi and colleagues’ analysis, with data on each ultimately favouring first-line aspiration thrombectomy. Patients in the aspiration group—as compared to those in the stent retriever group—experienced lower rates of vessel perforation (0.4% vs 0.8%), vessel dissection (0.7% vs 1.4%), emboli to new territory (0.6% vs 1.4%), and vasospasm (0.4% vs 1.4%). However, vasospasm was the only outcome that displayed a statistically significant difference between the two cohorts.
“Given the narrower therapeutic margin of thrombectomy for MeVO stroke, outcomes in these cases may be more sensitive to procedural variables—such as device selection, catheter size and trackability, procedure times, and device-related procedural complications like SAH, dissection and vasospasm—which may have less influence on the clinical outcome/natural history of thrombectomy patients with LVO [large vessel occlusion],” Majidi told the SNIS 2025 audience. “Therefore, future RCTs [randomised controlled trials] evaluating thrombectomy in MeVO must not only ensure rigorous patient selection—they should also place significant emphasis on the technical nuances of the procedure.”
Potential discrepancies between the outcomes that can be achieved with stent retriever- versus aspiration-first thrombectomy techniques—not only within MeVOs, but across ischaemic stroke more generally—are a topic of continued debate in the neurointerventional arena.
Regarding MeVO strokes specifically, a 2023 systematic review and meta-analysis published in the European Stroke Journal utilised data on nearly 1,900 patients in order to compare the two techniques. Investigators ultimately concluded that there is potential for efficacy- and safety-related benefits with stent retriever/primary combined techniques compared to aspiration-only approaches, citing higher odds of functional independence and lower odds of mortality with the former. Their data also suggested significantly higher odds of successful recanalisation when using a stent retriever only versus an aspiration catheter only, leading them to highlight the need for subsequent trials further assessing the possible advantages of utilising stent retrievers in more distally located occlusions.
Several other published pieces of research, including a 2022 subanalysis of the TOPMOST study in Stroke, and a 2023 propensity-score matched analysis from the MAD-MT consortium in Stroke: Vascular and Interventional Neurology, have found similar clinical and imaging-related outcomes between stent retriever- and aspiration-first approaches, reinforcing the importance of more high-level evidence on how the two techniques compare.