How did you come to choose medicine as a career and, in particular, what drew you to neuroscience and neuromodulation?
I chose medicine in part because my father was an MD and my youth was spent in this type of culture, constantly related to being concerned with patients and hearing that the doctors could help them. I was driven to neurosciences because it was so clear from different sources, even from books, and movies, and stories which I read, saw, and heard when I was a teenager, that there was almost nothing more interesting, except the universe itself! The interest in neuromodulation came progressively while performing neurosurgery, as it was suggested from basic teaching that the brain was a very complicated machine, able to receive and process data as well as creating orders capable of redefining the neurons. The concept of having these kinds of complex feedback loops contained in itself the idea that something could modulate neuronal activity in the brain and then the therapeutic tools which were used could be of this kind of neuromodulating tools.
Who were your mentors in the field and what do you still remember from their wisdom?
My mentor was essentially Professor Jacques de Rougemont whom I joined when I was an undergraduate medical student, and with whom I did my medical thesis, which was already research oriented (mathematical modelling of intracranial pressure). He was at the same time not only my teacher and mentor in neurosurgery, but also had a very strong influence on my vision in life and he transmitted, in addition to what I had already, a strong interest in the research lifestyle by simply accepting that an intern in neurosurgery could spend some of his time thinking about models of intracranial pressure and doing experiments on animals in his lab.
He was very demanding, considering it normal for us to be with him almost constantly in the hospital, at the bedside, in the operating room and also in the lab. He would often have us, his small team, around him for lunch or some Saturday evenings. I actually spent more time with him than with my own father.
His teaching was made of basic neurosciences, neurology, anatomy and surgical techniques. But he also taught what attitude we should have in front of patients and their family—to have as a primary concern the efficiency of our procedures, how this would be explained to the patients and how it was tolerated by them. He had been trained in neurosurgery in the States with William Sweet in Boston at Massachusetts General Hospital, where he learned, among many things, that the outcome was the goal, that speed had nothing to do with being a good neurosurgeon. He used to reconsider everything during surgery to look for another method. At that point as a student I had the feeling that there was no normal and established neurosurgical practice, until I realised that it was just my perception of his constant quest for a different, at least a better way, to operate.
Additionally, Jacques de Rougemont introduced me to Jean Talairach, a psychiatrist who reinvented stereotaxy and created a worldwide known atlas, as well as a stereotactic frame, demonstrating that the academic world should ignore frontiers. I spent a month in his department where I learned more than what could be found in a textbook, he was the textbook.
What was your most memorable case and why?
When you are a student and even a fellow, you have to learn everything, and quite often everything is memorable. Out of many situations, I have always been impressed by Professor Jacques de Rougemont’s patience, by his keeping extremely calm—when things were becoming critical, and the more stressing they would be, the more he would get in control. For instance, I remember very clearly how he managed to remove totally an anaplastic meningioma, which would bleed as soon as touched. He went on, resected it, controlling the bleeding until haemostasis was done, without having looked at the clock. He used very often small jokes such as when I was talking about the duration of the surgery and how he could keep going on with that, he would tell the story of the boy asking his father how far were the United States and the father would answer: “Shut up and keep swimming!”
What innovations have changed neuroscience and in particular, neurosurgery, in the last 20 years?
The second half of the century was totally dominated by the permanent production of novelties, such as general anaesthesia, electrocoagulation for haemostasis, radiology and very soon computerised radiology. I remember in 1972 the first picture of a haematoma provided by an EMI scanner: it changed the neurosurgical practice. For instance, the evacuation of a haematoma is such a simple procedure today, but at that time it was quite often a nightmare for the neurosurgeon who moved to the brain seeking a cavity filled with blood, sometimes not even being sure that there was a collection and that the displacement of the vessels as shown by angiography was not only a brain swelling that you could not evacuate.
You are regarded as the “father of high frequency deep brain stimulation”. Can you tell us about your discovery?
I like to say that I did not discover deep brain stimulation, which existed since about the 50s, but that I did invent deep brain stimulation at high frequency (meaning around and above 100Hz instead of the 30Hz previously used). This is what the true core of the invention is, and this was discovered under the principle of serendipity, meaning that you pay attention to an event which may have been already observed by others who left it unnoticed or not considered as important, because the observer at that time was not permanently thinking about your problem, while you catch the event because quite often your prepared mind recognises it as the expected solution it was looking for during its quest triggered by the problem.
Then, in 1987, during a thalamotomy to treat essential tremor, I was checking the location of the probe to be used for coagulation of the thalamic target, the ventral intermedius nucleus at that time. For this I used the classical method available at the time, which was electrical stimulation, usually at low-frequency, around 30Hz to 50Hz, to excite the tissue and avoid the misplacement if stimulation would elicitate dysesthesias (corresponding to the sensory thalamus where the lesion would create a loss of sensitivity and then intractable pain), or muscular contractions (these corresponding to the internal capsule where the lesion would induce a motor deficit). At a certain level, I observed unexpectedly that the tremor was suddenly arrested, when the stimulation was performed at a frequency close to 100Hz, and would recur instantaneously when it was turned off. This paradoxal effect, reproducible, was intriguing as the contrary (exacerbation of tremor or lack of effect) could have been expected or considered as normal. I thought it could be the solution I was looking for to replace the lesioning methods the complications of which were irreversible. The last 27 years have proven that it was a very satisfactory new method which is now used worldwide and has been extended to several other indications than Parkinson’s disease and movement disorders.
How do you see the field of neuromodulation developing in the future?
The future has started as soon as the method was applied first, extending to various new indications, providing new and safer treatments for a larger number of indications, and at the same time proving further the concept. Particularly, the possibility to perform again psychosurgery with reversible effects and non-permanent side effects and complications is in itself a revolution. It is up to us to use it wisely and not going to malpractice which was responsible for the moratorium of the 70s. The other branch of the future is in the understanding of the mechanism which is still unclear, probably corresponding to the multiple actions of several mechanisms, all of them leading to “functional inhibition”.
Another aspect of the future development is breaking the wall of neuroprotection which is the real thing of the disease. New issues are in progress such as near infrared illumination that we are developing.
What advice would you give to someone starting their career in neuromodulation?
Don’t do that! Neuromodulation is a method, not a whole discipline by itself. It has, as for functional neurosurgery at large, to be surrounded by the other methods of neurosurgery, to be able to evolve fruitfully. Even more, a method is doomed to be replaced by an even better one, and it is not wise for a young beginner to risk to be overcome by history.
What are your current areas of research focused on?
I am retired, and now the chairman of the board of Clinatec, devoted to developing innovative solutions for diagnosis and treatment in medicine. My own current topics in research are neuroprotection methods using near infrared illumination of the Substantia Nigra, new development of methods to improve deep brain stimulation, and brain computer interfaces to drive robotic exoskeletons for tetraplegic patients.
What new techniques/technologies are you keeping your eye on?
I believe gene therapy is still in development and preliminary results are encouraging. After all, this might be the ultimate therapeutical solution: restoring the production of dopamine in a dopamine deprived system.
In the meantime, micronanotechnologies and computing science are sources of high potential developments for improvement and diversification of deep brain stimulation towards new horizons.
What are your interests outside of medicine?
My interests outside of medicine include astronomy, cosmology, the evolution of the Universe, science fiction, opera music, Bernini statues, snorkelling and a little bit of golf.
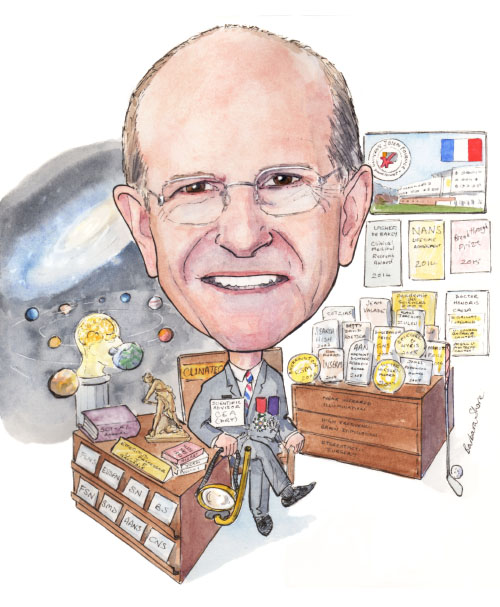
Fact file
Current position
Member of the Academy of Sciences and Scientific Advisor at the Commissariat à l’énergie atomique et aux énergies alternatives, Campus MINATEC, Grenoble, France
Education and career
1970 – Medical doctor
1978 – Doctor of Science (Physics)
1978–1984 – Professor of Experimental Medicine
1989–2004 – Head of the neurosurgery department of the University Hospital of Grenoble, France
1984–2007 – Professor of Biophysics at the University Joseph Fourier in Grenoble, France
1988–2007 – Director of the National Institute of Health and Medical Research (Inserm) Preclinical Neurosciences Unit
2007– – Scientific Advisor at CEA (the Technological Research Branch)
Societies
- Member of the French language Neurosurgical Society
- Member of the European Society for Stereotaxy and Functional Neurosurgery
- Member of the Society for Neuroscience
- Member of the Biophysical Society
- Member of the French Society for Neuroscience
- Member of the Society for Movement Disorders
- Member of the American Association of Neurological Surgeons
- Member of the Congress of Neurological Surgeons
Honours and awards (selected)
- Doctor Honoris Causa from the University of Galway (Ireland), University of London (Canada), McGill University, Montreal (Canada)
- Spiegel and Wycis Medal (2005)
- Matmut prize of medical innovation and the Foundation of the Future (2006)
- James Parkinson Award (2007)
- Victor Horsley Award (2007)
- American Academy of Neurology’s Movement Disorders Research Award (2008)
- Knight of the Academic Palms
- Knight of the Legion of Honour
- Lasker DeBakey Clinical Medical Research Award (2014)
- NANS Lifetime Achievement Award (2014)
- Breakthrough Prize in Life Sciences (2015)










