Data from a new study that maps out the levels at which adverse postoperative events decrease following transfemoral carotid artery stenting (TfCAS) based on depth of physician experience with the procedure represent an “absolute minimum threshold of learning”, according to the lead author.
This analysis comes in the wake of the US Centers for Medicare & Medicaid Services (CMS) decision to expand coverage for carotid stenting procedures and, in doing so, loosen restrictions on the use of TfCAS.
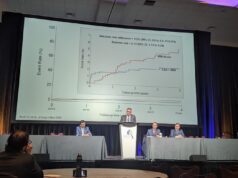
Findings from an analysis of the Society for Vascular Surgery’s (SVS) Vascular Quality Initiative (VQI)—which were presented at the 2024 Society for Clinical Vascular Surgery (SCVS) annual meeting (16–20 March, Scottsdale, USA)—showed that the number of procedures a physician had to perform in order to get an in-hospital stroke and death rate below 4% in symptomatic patients was 235. Similarly, to achieve a stroke and death rate below 2% in asymptomatic patients, the threshold physicians had to reach to derive benefit was 13 procedures.
Rates were based on the fact the best available VQI registry data relate to in-hospital stroke and death, not the 30-day stroke and death thresholds of 6% and 3% for symptomatic and asymptomatic patients, respectively.
Marc Schermerhorn (Beth Israel Deaconess Medical Center, Boston, USA), the study’s senior author, raised concerns over how the recent CMS coverage expansion will interplay with data reporting and, ultimately, the tracking of stroke and death rates going forward. “Now that CMS has done away with all the regulations and restrictions on who can do [TfCAS] procedures, where [they can do them] etc., people may not submit data to VQI anymore, unfortunately,” he said.
“There have been a lot of other studies that have shown transfemoral stenting outcomes are not as good as TCAR [transcarotid artery revascularisation] and CEA [carotid endarterectomy], but I think the concern now is, by opening up the doors for anybody to do carotid stenting, there could be a lot of people who have never done carotid stenting before who now decide to get into the game.
“I think that the way things were before, when you had to be an approved centre and you had to have credentialing committees that had to collect data, monitor that local data, and submit it to Medicare, that prevented a lot of people from doing the procedure. So, it concentrated in the people who have the most experience.”
However, the respective thresholds for symptomatic and asymptomatic cases represent the basement of learning, in Schermerhorn’s view.
“You have to remember that transfemoral stenting has been around since the turn of the century—and even before that,” he continued. “The VQI didn’t start collecting data on carotid stenting until 2005, and that was only in New England. It wasn’t until 2011 that we started to collect national data. So, most people who were in the carotid stent registries in the VQI had experience before they started submitting data, and so we actually don’t think this is a full representation of the learning curve.
“We know almost certainly most people had been doing cases prior to entry of data into the VQI, so this is an absolute minimum threshold of learning curve, and the true learning curve is likely larger. I don’t know how much, but it’s higher numbers.”
Schermerhorn said that, with the possibility of “a lot more novices” performing TfCAS in the wake of CMS coverage expansion, his team’s latest study clearly demonstrates “results are highly dependent on experience”.
Even supposing a lot of TfCAS experience, he went on to state that “the results don’t seem to be as good as with either TCAR or endarterectomy”.
Despite the potential for TfCAS entries into the VQI registry to decrease, Schermerhorn expects monitoring to continue, including via administrative databases, albeit with a lower level of clinical detail available, but expressed hope enough interest would persist in submitting data to the VQI.
“That’s my other concern,” he noted. “The people who are interested in submitting data are probably the ones who are more committed to quality improvement and striving toward knowing what their outcomes are—and improving them.”
That raises another dimension of the study presented at SCVS 2024, noted Schermerhorn: the research team also looked at whether those who had bad outcomes when they first started doing procedures were less likely to continue performing TfCAS. They found that this was indeed the case.
“The people who went on to do more than 25 procedures had better outcomes than the people who quit at up to 25 and then didn’t do any more,” he said.
“We presume that there is some feedback to people and that, if they’re finding that their own results are not that good, then they don’t continue to do the procedure. If people don’t track their outcomes somewhere, then they may not know.
“That’s the problem. When you have a procedure with a low adverse outcome event rate, it’s hard for people to gain personal perspective.”
Further concerns
Reservations over the CMS’ expansion of coverage for TfCAS have also been expressed recently by SVS president Joseph Mills (Baylor College of Medicine, Houston, USA), who told Vascular News that “this decision will likely increase the number of strokes in the USA in the near future”.
“Unrestricted access to TfCAS can be predicted to result in an increase in the number of operators performing the procedure at a low annual rate, slowly making their way through the learning curve, and struggling to achieve annual procedure numbers, with less-than-acceptable results for Medicare beneficiaries,” Mills stated.
“We believe the [CMS] decision was premature, especially given that the taxpayer-funded CREST-2 trial is not yet completed and may well shed important insights on the issue of who benefits from carotid revascularisation by stenting versus CEA compared to best medical therapy.”