A new study, published in the Journal of NeuroInterventional Surgery (JNIS) late last year, has assessed the safety of the latest iteration of the Pipeline Vantage embolisation device (Medtronic) in the treatment of unruptured intracranial aneurysm patients—ultimately producing “acceptable outcomes” with the technology.
The PEDVU study’s authors—led by Thomas Booth (King’s College Hospital NHS Foundation Trust, London, UK)—further report that this second, updated version of the Pipeline Vantage appears to boast superior efficacy and a similar safety profile in treating unruptured aneurysms, as compared to previous generations of the device.
“It is always vital to assess new devices in the clinic to assess and compare how effective they are in treating the disease, and how safe they are for the patients,” Booth said. “Overall, these are acceptable outcomes in this pragmatic and non-industry-sponsored study.”
Using data from eight hospitals, researchers based across the UK were able to show that the second version of the Pipeline Vantage could effectively and safely stop blood flow into patients’ unruptured aneurysms—as well as demonstrating that prior challenges regarding device placement had been overcome.
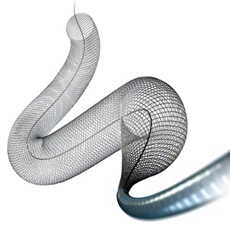
The first version of Medtronic’s Pipeline Vantage was introduced via a limited, premarket release. However, operators experienced technical difficulties when placing the device into an artery, leading to its withdrawal from the market. The second version was released globally following modifications to address these technical difficulties but, until now, had not been assessed clinically to confirm that said difficulties had been remedied.
Researchers therefore undertook a multicentre study with retrospective and prospective elements, analysing outcomes from eight UK centres using core laboratory assessments. They evaluated 30-day and ≥3-month mortality and morbidity rates, and six- and 18-month radiographic aneurysm occlusion rates, for procedures performed between July 2021 and March 2023. Primary and secondary objectives of their study were to determine outcomes for unruptured and ruptured aneurysm cohorts, respectively.
“We included 121 consecutive patients with 131 aneurysms,” the researchers write in JNIS, relaying their results. “The adequate occlusion rate for the unruptured cohort at short-term and medium-term follow-up, and also for the ruptured cohort at short-term follow-up, was >90%. Two aneurysms (1.5%) underwent retreatment. When mortality attributed to a palliative case in the unruptured cohort or subarachnoid haemorrhage in the ruptured cohort was excluded, then the overall major adverse event rate in respective cohorts was 7.5% and 23.5%, with 0% mortality rates for each. When all event causes were included on an intention-to-treat basis, the major adverse event rates in respective cohorts were 8.3% and 40.9%, with 0.9% and 22.7% mortality rates.”
Among other conclusions drawn by the researchers is this second version of the Pipeline Vantage appearing to be easier to deploy compared to its predecessor, in addition to suggestions of superior efficacy and an equivalent safety profile for unruptured aneurysms.
While their deductions regarding ruptured aneurysms are “limited” by a small cohort size within the present study, the researchers report observations of efficacy that are similar to previous studies and “may be acceptable”. However, they add that there appears to be a high rate of adverse events in these acute and typically riskier cases—and, as such, evidence from further, prospective outcome studies is needed to justify the routine use of Pipeline Vantage embolisation devices in ruptured aneurysms.









