This advertorial is sponsored by Medtronic.

© 2024, November Medtronic, Inc. REPRINTED WITH PERMISSION-ALL RIGHTS RESERVED
As the co-founder and chief executive officer of Chestnut Medical, Aaron Berez played a leading role in bringing flow diverters to market with the development of the Pipeline embolisation device (Medtronic) for intracranial aneurysm treatment. Today, his main focus is somewhat different, as he and his colleagues at Alembic seek to raise the bar in neurovascular catheter technology, but Berez ultimately remains in a similar position—attempting to drive innovation in the neurointerventional space forward once more.
“Catheter designs are always a balance between making something that is very soft, flexible and easily trackable but, on the other hand, robust enough that it can withstand usage and perform well,” Berez tells NeuroNews. “And I have a bias towards making something that is easy to use and tracks well because, if it is not, no one is ever going to use it and they will not find out how good it is.”
Casting an eye over the current marketplace of aspiration catheters for mechanical thrombectomy, Berez points out that many existing technologies do offer a high level of trackability and, thus, are used widely by physicians. However, he continues, these same catheters are “not very durable or robust”, and this can lead to problems, for example, when deploying them in combination with a stent-retriever device due to the increased degree of friction this combined technique creates.
“Stent retrievers, in general, are being used less, but they are still used in a fair number of cases,” Berez asserts, also noting that somewhere between one-third and one-half of all centres still employ these devices in their thrombectomy practices.
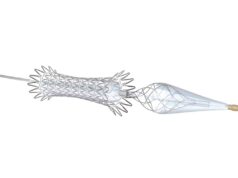
As such, with APRO®—a technology being distributed by Medtronic since 2023—Berez and the Alembic team sought to develop a catheter that would offer comparable trackability to today’s gold standard, but would simultaneously be robust enough to maintain its shape during use; would not collapse while aspirating; and could be used in conjunction with ancillary devices like stent retrievers.
Key features
Berez notes multiple characteristics of the APRO catheter that, in his view, enable it to achieve this overarching goal. The first feature he draws attention to is a “lubricious liner” material on the device’s surface that extends all the way to the tip of the catheter. The key benefit of this, according to Berez, is that it promotes improved interaction with stent-retriever devices, and thus is well-suited to physicians who favour a combined thrombectomy approach whereby an aspiration catheter is deployed in conjunction with the SolitaireTM revascularisation device (Medtronic) or an alternative stent retriever.
He also details the “extensive length” of hydrophilic coating on the APRO device, which reduces friction and makes the catheter’s surface “glide” across the blood vessels while it is being deployed and advanced.

“What that means is the force that you have to apply to advance the catheter is reduced, making it easier to advance and putting less stress on the vessel,” Berez clarifies.
He further notes that the reinforced construction and design of the device with braids, coils and polymers allows it to resist “ovalisation” and kinking while traversing bends in the patient’s vasculature, and maintain its shape under aspiration force as well.
Touching on the different iterations of the device that are either currently or soon-to-be available, Berez states that the largest catheter in the APRO family—the APRO 70, which has an inner diameter of 0.07 inches— is already on sale in the USA, having gained Food and Drug Administration (FDA) clearance late last year. Smaller sizes are in the works, he continues, with APRO 55 having been submitted to the FDA and US clearance anticipated at the beginning of 2024 and an even smaller version of the catheter not far behind.
“What we are trying to do is provide physicians with catheters that are easy to use, and can be used together to treat a wide range of intracranial occlusions—from small vessels in the periphery [of the neurovasculature] to large vessels like the MCA [middle cerebral artery], and even larger vessels like the ICA [internal carotid artery],” Berez adds. “The goal of aspiration thrombectomy is to re-establish flow quickly and safely, and APRO can do that. And, in properly selected patients, that can result in less brain damage and smaller infarct sizes.”
APRO tailored to “effective” combined approach in stroke thrombectomy
“I typically use combination therapy, which means pairing SolitaireTM [Medtronic] with an aspiration catheter, and I do so because I think it is the most effective way of extracting a clot in the setting of acute ischaemic stroke,” says Daniel Sahlein (Goodman Campbell Brain and Spine, Indianapolis, USA), providing NeuroNews with a snapshot of his paradigm for mechanical thrombectomy procedures.
To support this statement, Sahlein draws on his team’s “very large” interventional stroke practice— which, at time of writing, is on pace to perform roughly 300 thrombectomies across all of 2023.
“We have tried many different techniques, and we feel that combination therapy works best,” he says. “We are doing an average of six thrombectomies a week— which means we are doing up to 10 or 15 in some weeks—and we can really see, with our own eyes, the difference in efficacy between the different techniques.
“Combination therapy, I think, works best, and the technique that works best to cleanly extract a clot also leads to better clinical outcomes—and there is overwhelming evidence to support this contention. So, that is the strategy that I personally favour.”
Here, Sahlein cites the five major randomised controlled trials, published in 2015, that helped to establish the superior efficacy of mechanical thrombectomy over standard medical care at the time. These trials all saw the Solitaire revascularisation device being used to deliver the majority of thrombectomy treatments.
Subsequent studies have indicated that “good recanalisation” is achievable via an aspiration-only approach but, he stresses, these outcomes are still inferior to those demonstrated when a stent retriever and an aspiration catheter are deployed in tandem. And, according to Sahlein, while COMPASS and ASTER both found broadly similar outcomes between stent retriever- and aspiration-only approaches, a closer look at more granular data from these studies reveals some “compelling” pieces of evidence supporting combination therapy as well.
In COMPASS, he explains, some 15% of stent retriever-first cases did use concomitant aspiration, which Sahlein feels is “a lot” given the potential benefits of combining the two techniques. In addition, 21% of patients in COMPASS’ aspiration-first arm ended up using a stent retriever in subsequent passes—with all of these using aspiration with the stent retriever or a “true” combined approach.
 Although ASTER reported equivalent clinical outcomes between its stent retriever- and aspiration-first arms, Sahlein highlights that modified Rankin scale (mRS) 0–2 rates were roughly 5% higher with a stent retriever. He also points out that this superiority was achieved despite the stent-retriever group potentially being “hamstrung” by having 6% more carotid terminus occlusions—technically challenging cases typically associated with worse clinical outcomes—than the aspiration group. Sahlein avers that evaluations of aspiration-only compared to combination therapy found a 5% higher rate of good recanalisation with the latter technique when looking at technical efficacy after first-line treatment alone (using cohort-assigned thrombectomy technique only versus first pass with subsequent potential crossover). Overall analyses of these data reveal technical success outcomes that “tip towards use of a stent retriever”, he notes, with clinical outcomes leaning even more heavily toward favouring stent-retriever usage. “I think that use of Solitaire really augments and improves aspiration in many ways, and does not detract in any way,” he adds.
Although ASTER reported equivalent clinical outcomes between its stent retriever- and aspiration-first arms, Sahlein highlights that modified Rankin scale (mRS) 0–2 rates were roughly 5% higher with a stent retriever. He also points out that this superiority was achieved despite the stent-retriever group potentially being “hamstrung” by having 6% more carotid terminus occlusions—technically challenging cases typically associated with worse clinical outcomes—than the aspiration group. Sahlein avers that evaluations of aspiration-only compared to combination therapy found a 5% higher rate of good recanalisation with the latter technique when looking at technical efficacy after first-line treatment alone (using cohort-assigned thrombectomy technique only versus first pass with subsequent potential crossover). Overall analyses of these data reveal technical success outcomes that “tip towards use of a stent retriever”, he notes, with clinical outcomes leaning even more heavily toward favouring stent-retriever usage. “I think that use of Solitaire really augments and improves aspiration in many ways, and does not detract in any way,” he adds.
Sahlein’s stent retriever of choice for this combined approach is Solitaire—a well-established industry leader that played a pivotal role in cementing thrombectomy as a new standard of care in selected stroke patients. However, APRO® (Medtronic)—the aspiration catheter he prefers to use in conjunction with Solitaire—is more of a newcomer on this particular scene.
He details that he has been using APRO catheters since July 2023, integrating them into his thrombectomy practice almost immediately after it became available in the USA earlier in the year. Discussing the key benefits of the device, Sahlein avers that it offers a level of trackability that places it in “the elite tier of catheters”, but that “it is a little bit more robust than those other offerings” as well.
“This [robustness] helps in more than one way,” he continues. “One of them is if you are going to pair it with Solitaire, and another one is the fact that, under maximal negative pressure, some of these catheters actually have a tendency to collapse slightly—and you can even see that at the proximal end of the catheter during a case.”
According to Sahlein, the robustness of APRO makes it less susceptible to these potential difficulties, firstly by enabling it to resist negative pressure and maintain its full luminal diameter—which helps with flow and clot extraction—but also via the aforementioned ability to pair it with Solitaire.
“At this point, there are a number of tools [in stroke thrombectomy] that are more on the commoditised side of things; they are all fairly similar in terms of performance, and within the same class,” Sahlein concludes, outlining the thought process that led him to choose APRO in the first place. “And so, for me personally, I choose in part based on who I would like to partner with and who I think represents best-in-class in terms of their commitment to serving neurovascular patients; their commitment to investing in research to move the field forward; and in terms of their current portfolio. I see Medtronic leading in all of these areas in their neurovascular work and so, all things [being] equal, if you have a tool that falls into a category that is a little more commoditised, selecting this tool based on who you desire to partner with in this space, I think, is a great way to go about doing things.”
Why “consistent and reliable” APRO catheter is well-suited to aspiration-first thrombectomy
Paying mind to current debates surrounding the benefits of stent retrievers, aspiration catheters, or a combination of the two, in the treatment of acute ischaemic stroke patients, Michael Chen (Rush University Medical Center, Chicago, USA) discusses why he prefers the aspiration-first approach—and chooses to deploy the APRO® catheter in his thrombectomy practice.
Why is ADAPT your chosen first-line technique when it comes to thrombectomy?
As outlined in the paper describing ADAPT [A Direct Aspiration First Pass Technique], published nearly 10 years ago in the Journal of NeuroInterventional Surgery by Turk et al, the initial primary advantages were speed, safety and cost. Effectiveness was still modest at the time, with a <50% rate of first-pass effect. Since then, there have been significant improvements in catheter trackability—at the distal tip, the transition zones, the hydrophilic coating and proximal support to help track around tortuous vessels, and move past edges caused by branch origins, such as the ophthalmic artery. Future iterations include different aspiration forces being applied, and compatible guide catheters that track as high as the cavernous carotid or higher, all promise to improve the rate of first-pass complete reperfusion. Personally, I prefer hydrophilic catheters to be the primary contact with the endothelial cell wall rather than a nitinol laser-cut stent with outward radial force.
What characteristics do you look for in an aspiration catheter?
Although much of the recent design iterations have focused on increasing the size of the inner lumen diameter to maximise aspiration force, the bigger challenge has been balancing this feature with catheter trackability. The construction of the catheter wall, with or without certain liners, hydrophilic exteriors, and use of braiding, are among the elements that have undergone iterations. All of this adds up to query whether it is possible, after positioning the tip of the aspiration catheter at the proximal face of the clot, for the catheter to then be independently advanced under aspiration to envelop the entire length of the clot. The one performance characteristic that captures all the essential design elements, to me, is whether—after positioning the catheter tip at the mid-M1 segment—it can then be advanced under aspiration, by itself, to the dominant M2 branch. Truth be told, particular guide catheters that can be placed distally, such as near the cavernous segment, greatly help the performance of aspiration catheters.
 What are your clinical experiences with the APRO catheter to date?
What are your clinical experiences with the APRO catheter to date?
My first-hand clinical experiences with the APRO catheter to date have been favourable. I do take the time to hydrate the exterior of the catheters by either letting them sit in a bowl of saline for a couple minutes or wiping them down several times with a wet Telfa dressing. A good sign of a highly trackable, hydrophilic catheter surface is one that is very slippery as you are trying to advance it into the rotating haemostatic valve of the guide catheter—which I have certainly noticed with APRO. The trackability seems consistent and reliable. I have also used it in conjunction with a stent retriever and encountered no issues with any deformation of the catheter tip. Although, as per instructions for use (IFU), it is recommended to be used with microcatheter, I have also been advancing the APRO catheter with larger 0.035-inch neurovascular guidewires alone to gain intracranial access.
Why did you opt to switch to APRO in your practice?
I think the performance of the Sofia aspiration catheter [Microvention/ Terumo] proved the value of high trackability with these devices. It is reassuring to know that the APRO catheter is tested and able to achieve high trackability while maintaining sufficient structural integrity after multiple stent-retriever passes.
DISCLAIMERS:
SolitaireTM is a trademark of Medtronic, Inc.
PhenomTM is a trademark of Medtronic, Inc.
APRO® is a registered trademark of Palmera Medical and is manufactured by Alembic LLCTM. The APRO catheter is currently only cleared and available in the USA.
Indications, contraindications, warnings and instructions for APRO® 70 Catheter can be found in each device package. Indications, contraindications, warnings and instructions for use for all other products can be viewed at www.medtronic.com/manuals.