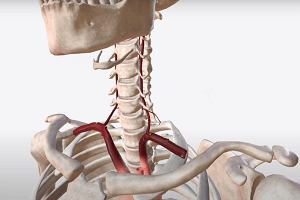
Stenting is something that, for now at least, should be considered in the extracranial vertebral arteries only—and not the intracranial arteries—for symptomatic atherosclerotic stenosis, as indicated by a majority vote from attendees at the Charing Cross (CX) 2021 Digital Edition (19–22 April, online).
After hearing arguments from either side of this controversial topic, mainly regarding the potential safety risks and clinical benefits associated with intracranial artery stenting in stroke patients, 64% of the CX audience voted in favour of the motion that ‘Only extracranial, not intracranial, vertebral arteries should be considered for stenting’.
The debate saw Andrew Clifton (St George’s University Hospitals NHS Foundation Trust, London, UK) start by presenting in favour of this motion. Clifton chose to focus on VIST (Vertebral artery ischaemic stenting trial)—a study that compared vertebral angioplasty and stenting plus best medical treatment (BMT) with BMT alone in 182 patients, and concluded that stenting may be effective in reducing stroke risks, predominantly in extracranial vertebral artery stenosis patients. VIST also found no strokes or major complications in 48 patients who underwent stenting for extracranial stenosis, while two strokes—one of which was fatal—were observed in 13 intracranial stenosis patients.
Clifton went on to expand his argument to include two further relevant clinical trials, namely VAST (Vertebral artery stenting trial) and SAMMPRIS (Stenting versus aggressive medical management for preventing recurrent stroke in intracranial stenosis), pooling data from 354 patients across all three studies to assert that “some benefit” in stroke prevention was observed for extracranial stenting, but not for intracranial stenting, as well as a “marked” periprocedural risk of stroke and death associated with the latter.
He finished his presentation by claiming neither extracranial nor intracranial stenting strategies have been shown to provide a statistically significant benefit in stopping recurrent stroke. Clifton followed this by adding that—while larger trials may reveal a more tangible benefit in extracranial stenting—he “can only advocate stenting of symptomatic, extracranial vertebral stenosis within 14 days of a transient ischaemic attack or posterior circulation stroke, and only in the context of a randomised trial”, but “cannot advocate” stenting for intracranial stenosis.
The riposte to Clifton’s argument was then provided by Thomas Liebig (Ludwig Maximilian University of Munich, Munich, Germany), who began his argument against the motion by saying he believes extracranial versus intracranial stenting “should not be the question”, but that treatment choices should depend on the individual patient’s anatomy. And, while he conceded there is little existing evidence on rescue stenting, Liebig referenced the Chinese study entitled ‘Efficacy and safety of rescue stenting following failed mechanical thrombectomy for anterior circulation large vessel occlusion: propensity score analysis’, which was published in the Journal of NeuroInterventional Surgery (JNIS) last year and found the survival rate in acute stroke patients receiving rescue stenting was “almost double” that of patients who did not.
Liebig went on to argue that advances in medical imaging technologies, such as quantitative magnetic resonance angiography (QMRA) and flat-panel computed tomography angiography (FP-CTA), have meant patients who require stenting can be identified more effectively—allowing clinicians to tailor their treatment strategies accordingly. When questioned by CX Executive Board member, and one of the session’s moderators, Hugh Markus (University of Cambridge, Cambridge, UK), over the fact that wider trials are needed to prove the benefits held by intracranial stenting, Liebig said he agreed “absolutely”, but added: “The point I was trying to make with my presentation is that it is generally not doing all patients a good service if you are very dogmatic about something, and are saying you should never do it.”
Later in the discussion, Clifton was also questioned by Markus on whether new stenting technologies could shed more light on intracranial, and indeed extracranial, stenting for stroke patients, and said: “Intracranially, yes, technology will make a big difference—and patient selection will make a big difference—but I think we have got to prove that extracranial works first, because the complication rates in the intracranial arms of all those previous trials were so high”. On the subject of future trials, Clifton and Liebig’s views were seemingly aligned, as Liebig added that, with the help of improved technology and better patient selection, “we might find patients that actually have more benefit than risk from doing these treatments”. Regarding the debate at hand, however, the CX audience ultimately sided with Clifton, voting in favour of the motion by a margin of 64% to 36%.
The CX debate on extracranial versus intracranial vertebral artery stenting can be viewed online here by registrants.