 A study comparing three different stents used during stent-assisted coiling of cerebral aneurysms revealed that the type of stent used affects a patient’s immediate and long-term health outcomes, while a significant difference in the rate of complete occlusion among the stents was found. Maxim Mokin (University of South Florida, Tampa, USA) presented these data at the Society of NeuroInterventional Surgery’s annual meeting (SNIS; 22–25 July, Miami, USA).
A study comparing three different stents used during stent-assisted coiling of cerebral aneurysms revealed that the type of stent used affects a patient’s immediate and long-term health outcomes, while a significant difference in the rate of complete occlusion among the stents was found. Maxim Mokin (University of South Florida, Tampa, USA) presented these data at the Society of NeuroInterventional Surgery’s annual meeting (SNIS; 22–25 July, Miami, USA).
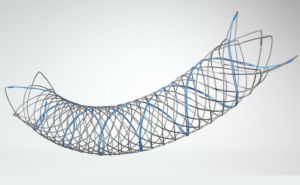
The multicentre analysis of radiographic and clinical outcomes in 659 patients with 670 cerebral aneurysms compared the angiographic and clinical outcomes of endovascular coiling using three types of stents—Neuroform (NEU; Stryker), Enterprise (EP; Codman Neuro, part of the DePuy Synthes Companies of Johnson & Johnson), and Low-profile Visualized Intraluminal Support (LVIS; MicroVention Terumo).
The majority (73%) were anterior circulation aneurysms, 19% were ruptured and 89% of treated aneurysms were considered wide neck, while 58% were medium sized aneurysms (5–15mm). According to Mokin, a variety of treatment approaches were used, as well as different configurations of devices, with “jailing” and “coil-through” being the most common stent deployment techniques, used 39% and 38% of the time, respectively. Coiling first and then deploying the stent was administered 10% of the time, while balloon-assisted coiling followed by stenting was used 13% of the time.
Yet, he said, “The weakest part of the study was that we had no core lab adjudication. Each centre adjudicated their own results.” Regardless, Mokin reiterated that dependent on the type of stent—there was a significant difference between the type of stent used and the degree of occlusion at immediate post-procedural outcome as well as at follow-up, with LVIS demonstrating superior angiographic results (p=0.0004).
“At follow-up, 84% of those treated with LVIS elicited a Raymond-Roy Grade Scale (RRGS) of 1. In comparison, 78% of patients treated with Neuroform and 68% of those treated with Enterprise achieved the same grade,” he said.
Furthermore, because the sample size was so large, the investigators were able to carry out subgroup analyses for both ruptured and unruptured aneurysms. “The significant difference seen in the type of stent and degree of occlusion; it remains in both ruptured and unruptured aneurysms when analysed separately,” Mokin remarked, adding that for unruptured aneurysms, the investigators also noticed that there was a significant association between the type of stent and procedural-related complications, such as intraprocedural rupture and in-stent thrombosis, which was higher in the LVIS group. However, he noted that there was no association in post-procedural complication rates of aneurysm recurrence, stroke, or stent stenosis based on stent type (p=0.76).
Lastly, Mokin alluded to whether there were any differences in the patterns of treatment at the six participating centres. “The data for this were highly significant. Every variable that we looked at elicited a p-value of <0.05. These included the type of stents used, the approach to stent-assisted coiling as well as angiographic outcomes—they were quite variable. It makes you wonder […] when you see the single centre studies or multicentre joint efforts, there is high variability between how each centre performs, and this should be accounted for.”
With this in mind, Mokin concluded by saying that randomised prospective trials comparing the different types of stents are warranted, and would be “a good next step to further improve clinical outcomes and safety”.













